YT: OUTLIVE by Peter Attia, MD | Core Message - YouTube
- Exercise
- Zone 2 trianing 4x45 mins / week
- Vo2 max trianing once a week: 4x 4min work, 4 min rest
- Strength training 3x per week
- Diet
- 1g protein per pound body weight
- 4 meals per day w/ 25% protein per meal
- Cut out refined carbs
Summary
Exercise is by far the most potent longevity "drug." No other intervention does nearly as much to prolong our lifespan and preserve our cognitive and physical function.
If you increase your muscle strength and improve your cardiorespiratory fitness, you have also reduced your risk of dying from all causes by a far greater magnitude than you could achieve by taking any cocktail of medications.
The data are unambiguous: exercise not only delays actual death but also prevents both cognitive and physical decline, better than any other intervention.
The best science out there says that what you eat matters, but the first-order term is how much you eat: Next is sleep, which I and many others had ignored for far too long.
When I look at a patient’s blood panel for the first time, my eyes immediately dart to two numbers: apoB and Lp(a).
Exercise is the only intervention shown to delay the progression of Parkinson’s.
"Being unfit carried a greater risk than any of the cardiac risk factors examined," the authors concluded.
Strength may even trump cardiorespiratory fitness, at least one study suggests.
About three hours per week of zone 2, or four 45-minute sessions, is the minimum required for most people
- The tried-and-true formula for these intervals is to go four minutes at the maximum pace you can sustain for this amount of time.
- Then ride or jog four minutes easy, which should be enough time for your heart rate to come back down to below about one hundred beats per minute.
- Repeat this four to six times and cool down.
- A single workout per week in this zone will generally suffice.
A far more important measure of strength, I’ve concluded, is how much heavy stuff you can carry.
- (A good goal is to be able to carry one-quarter to one-third of your body weight once you develop enough strength and stamina.
- Here we like to see men hang for at least two minutes and women for at least ninety seconds at the age of forty.
Conclusion: Stop overthinking nutrition so much. Put the book down. Go outside and exercise.
All of this is highly individual; everyone responds and adapts to trauma in a unique way
Read Terrence Real’s book I Don’t Want to Talk About It, a groundbreaking treatise on the roots of male depression.
David Brooks’s book The Road to Character.
Practicing DBT means literally working through a workbook with a DBT therapist, doing exercises every day.
Another way in which mindfulness helps is by reminding us that when we are suffering, it is rarely because of some direct cause,
One obvious way this applies is in how we think about ourselves. What does our inner dialogue sound like? Is it kind and forgiving and wise, or is it harsh and judgmental,
Exposing oneself to the fractal geometric patterns in nature can reduce physiological stress, and that these effects show up on an EEG.
I complement my therapy sessions by writing in my journal, a place where I can practice articulating my emotions and understanding them, holding nothing back.
I feel strongly that there is no substitute for this kind of work with a trained therapist.
PART I
CHAPTER 1 The Long Game From Fast Death to Slow Death
There comes a point where we need to stop just pulling people out of the
river. We need to go upstream and find out why they’re falling in. -- Bishop
Desmond Tutu
The odds are overwhelming that you will die as a result of one of the chronic diseases of aging that
Four Horsemen:
- heart disease,
- cancer,
- neurodegenerative disease, or type 2 diabetes
- related metabolic dysfunction.
Exercise is by far the most potent longevity "drug." No other intervention does nearly as much to prolong our lifespan and preserve our cognitive and physical function.
CHAPTER 2 Medicine 3.0 Rethinking Medicine for the Age of Chronic Disease
The time to repair the roof is when the sun is shining. -- John F. Kennedy
Risk is not something to be avoided at all costs; rather, it’s something we need to understand, analyze, and work with.
Every single thing we do, in medicine and in life, is based on some calculation of risk versus reward.
Nearly all the money flows to treatment rather than prevention -- and
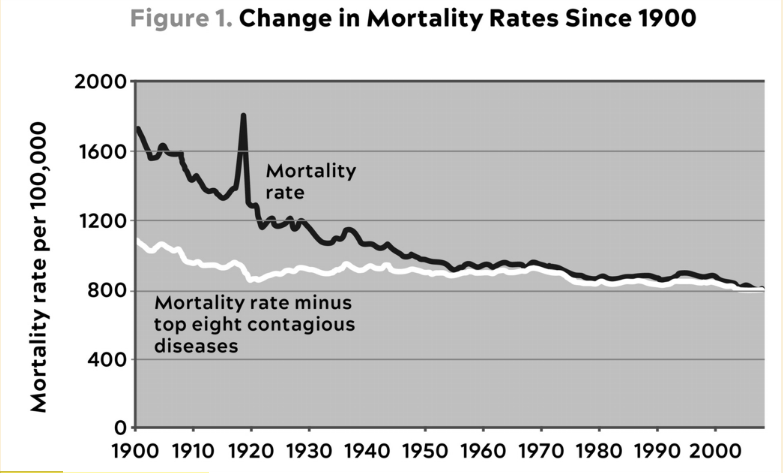 Source: Gordon (2016). This graph shows how little real mortality rates have
improved since 1900, once you remove the top eight contagious/infectious
diseases, which were largely controlled by the advent of antibiotics in the
early twentieth century.
Source: Gordon (2016). This graph shows how little real mortality rates have
improved since 1900, once you remove the top eight contagious/infectious
diseases, which were largely controlled by the advent of antibiotics in the
early twentieth century.
CHAPTER 3 Objective, Strategy, Tactics A Road Map for Reading This Book
Strategy without tactics is the slowest route to victory. Tactics without
strategy is the noise before defeat. -- Sun Tzu
Tactics are what you do when you are actually in the ring.
The strategy is the harder part, because it requires careful study of one’s opponent, identifying his strengths and weaknesses, and figuring out how to use both to your advantage, well before actually stepping in the ring.
Think about healthspan and its deterioration in terms of three categories, or vectors.
- The first vector of deterioration is cognitive decline.
- The second vector of deterioration is the decline and eventual loss of function of our physical body.
- familiarize yourself with something called the "activities of daily living,"
- a checklist used to assess the health and functionality of elderly people.
- The third and final category of deterioration, I believe, has to do with emotional health.
Surveys show that happiness tends to reach its nadir in our forties (age forty-seven, to be exact),
But as I learned through painful experience, middle-aged distress often has its roots much earlier, in adolescence or childhood.
If you increase your muscle strength and improve your cardiorespiratory fitness, you have also reduced your risk of dying from all causes by a far greater magnitude than you could achieve by taking any cocktail of medications.
Our tactics in Medicine 3.0 fall into five broad domains:
- exercise,
- nutrition,
- sleep,
- emotional health,
- exogenous molecules, meaning drugs, hormones, or supplements.
Break down this thing called exercise into its most important components:
- strength,
- stability,
- aerobic efficiency,
- peak aerobic capacity.
The data are unambiguous: exercise not only delays actual death but also prevents both cognitive and physical decline, better than any other intervention.
The best science out there says that what you eat matters, but the first-order term is how much you eat:
Next is sleep, which I and many others had ignored for far too long.
"Why would you want to live longer if you’re so unhappy?"
A one-year clinical trial, or even a five-year study, will not tell us everything we need to know about disease processes that take decades to unfold.
Mendelian randomization, or MR for short. MR helps bridge the gap between randomized controlled trials, which can establish causality, and pure epidemiology, which often cannot.
Mendelian randomization helps tease out causal relationships between modifiable risk factors (e.g., LDL cholesterol) and an outcome of interest (e.g., cancer) in situations where actual randomized experiments cannot easily be done.
PART II
CHAPTER 4 Centenarians The Older You Get, the Healthier You Have Been
Whiskey's a good medicine. It kees your muscles tender. -- Richard Overton
Studies of Scandinavian twins have found that genes may be responsible for only about 20 to 30 percent of the overall variation in human lifespan. The catch is that the older you get, the more genes start to matter.
Pursuing two approaches in parallel.
- think about very early disease-specific prevention,
- think about very early general prevention, targeting all the Horsemen at once, via common drivers and risk factors.
CHAPTER 5 Eat Less, Live Longer? The Science of Hunger and Health
Scientists who play by someone else’s rules don’t have much chance of making discoveries. -- Jack Horner
Rapamycin acted directly on a very important intracellular protein complex called mTOR (pronounced "em-tor"), for "mechanistic target of rapamycin."
MTOR? Because this mechanism turns out to be one of the most important mediators of longevity at the cellular level.
Not only that, but it is highly "conserved," meaning it is found in virtually all forms of life, ranging from yeast to flies to worms and right on up to us humans.
In biology, "conserved" means that something has been passed on via natural selection, across multiple species and classes of organisms -- a sign that evolution has deemed it to be very important.
The job of mTOR is basically to balance an organism’s need to grow and reproduce against the availability of nutrients.
When food is plentiful, mTOR is activated and the cell (or the organism) goes into growth mode,
When nutrients are scarce, mTOR is suppressed and cells go into a kind of "recycling" mode, breaking down cellular components and generally cleaning house.
The authors of the study, published in Nature, speculated that rapamycin might extend lifespan "by postponing death from cancer, by retarding mechanisms of aging, or both."
When resveratrol was subjected to the same sort of rigorous testing as rapamycin, as part of a National Institute on Aging program to test potential antiaging interventions, it did not extend lifespan in a similar diverse population of normal mice.
Study after study since 2009 has confirmed that rapamycin can extend mouse lifespans pretty reliably. It has also been shown to do so in yeast and fruit flies,
How much food we eat correlates somehow with how long we live.
Scientists have actually found that the less they feed the animals, the longer they live. Its effects seem to be dose dependent, up to a point,
It seems that, across the board, hungry animals become more resilient and better able to survive, at least inside a well-controlled, germ-free laboratory.
There is no evidence that extreme CR would truly maximize the longevity function in an organism as complex as we humans,
Reducing the amount of nutrients available to a cell seems to trigger a group of innate pathways that enhance the cell’s stress resistance and metabolic efficiency -- all of them related, in some way, to mTOR.
The first of these is an enzyme called AMP-activated protein kinase, or AMPK for short. AMPK is like the low-fuel light on the dashboard of your car:
While this typically happens as a response to lack of nutrients, AMPK is also activated when we exercise,
AMPK prompts the cell to conserve and seek alternative sources of energy.
It does this first by stimulating the production of new mitochondria,
Over time -- or with disuse -- our mitochondria become vulnerable to oxidative stress and genomic damage,
Restricting the amount of nutrients that are available, via dietary restriction or exercise, triggers the production of newer, more efficient mitochondria to replace old
These fresh mitochondria help the cell produce more ATP,
AMPK also prompts the body to provide more fuel for these new mitochondria, by producing glucose in the liver (which we’ll talk about in the next chapter) and releasing energy stored in fat cells.
More importantly, AMPK works to inhibit the activity of mTOR,
By cleansing our cells of damaged proteins and other cellular junk, autophagy allows cells to run more cleanly and efficiently and helps make them more resistant to stress.
Historically, rapamycin was approved to treat patients indefinitely following organ transplantation,
This immune-suppressing effect explains why there has been some reluctance to consider using (or even studying) rapamycin in the context of delaying aging in healthy people,
December 2014 with the publication of a study showing that the rapamycin analog everolimus actually enhanced the adaptive immune response to a vaccine in a group of older patients.
MTOR, which is actually composed of two separate complexes, called mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2).
The two complexes have different jobs, but (at risk of oversimplifying) the longevity-related benefits seem to result from inhibiting complex 1.
Giving the drug daily, as is typically done with transplant patients, appears to inhibit both complexes, while dosing the drug briefly or cyclically inhibits mainly mTORC1, unlocking its longevity-related benefits, with fewer unwanted side effects.
Senescent cells, which are "older" cells that have stopped dividing but have not died; these cells secrete a toxic cocktail of inflammatory cytokines, chemicals that can harm surrounding cells.
Rapamycin seems to reduce these inflammatory cytokines.
FDA has given the green light for a clinical trial of another drug with potential longevity benefits, the diabetes medication metformin.
Researchers noticed (and studies appeared to confirm) that patients on metformin appeared to have a lower incidence of cancer than the general population.
One large 2014 analysis seemed to show that diabetics on metformin actually lived longer than nondiabetics, which is striking.
What we eat and how we metabolize it appear to play an outsize role in longevity.
CHAPTER 6 The Crisis of Abundance Can Our Ancient Genes Cope with Our Modern Diet?
Avoidable human misery is more often caused not so much by stupidity as by
ignorance, particularly our ignorance about ourselves. -- Carl Sagan
More than one in four people on this planet have some degree of NASH or its precursor, known as nonalcoholic fatty liver disease, or NAFLD,
The first signs would generally show up only on a blood test for the liver enzyme alanine aminotransferase (ALT for short).
But not everyone who is obese is metabolically unhealthy, and not everyone who is metabolically unhealthy is obese.
"metabolic syndrome" (or MetSyn), and it is defined in terms of the following five criteria:
- high blood pressure (>130/85)
- high triglycerides (>150 mg/dL)
- low HDL cholesterol (<40 mg/dL in men or <50 mg/dL in women)
- central adiposity (waist circumference >40 inches in men or >35 in women)
- elevated fasting glucose (>110 mg/dL)
If you eat a doughnut, for example, the body has to decide what to do with the calories
- it can be converted into glycogen, the storage form of glucose, suitable for use in the near term.
- About 75 percent of this glycogen ends up in skeletal muscle and the other 25 percent goes to the liver,
An adult male can typically store a total of about 1,600 calories worth of glycogen between these two sites, or about enough energy for two hours of vigorous endurance exercise.
One of the liver’s many important jobs is to convert this stored glycogen back to glucose and then to release it as needed to maintain blood glucose levels at a steady state, known as glucose homeostasis.
An average adult male will have about five grams of glucose circulating in his bloodstream at any given time, or about a teaspoon.
That teaspoon won’t last more than a few minutes, as glucose is taken up by the muscles and especially the brain, so the liver has to continually feed in more,
Consider that five grams of glucose, spread out across one’s entire circulatory system, is normal, while seven grams -- a teaspoon and a half -- means you have diabetes.
We have a far greater capacity, almost unlimited, for storing energy as fat-- the second possible destination for the calories in that doughnut.
Even a relatively lean adult may carry ten kilograms of fat in their body, representing a whopping ninety thousand calories of stored energy.
That decision -- where to put the energy from the doughnut -- is made via hormones, chief among them insulin,
The twist here is that fat -- that is, subcutaneous fat, the layer of fat just beneath our skin -- is actually the safest place to store excess energy. Fat in and of itself is not bad. It’s where we should put surplus calories.
While fat might not be culturally or aesthetically desirable in our modern world, subcutaneous fat actually plays an important role in maintaining metabolic health.
The Yale University endocrinologist Gerald Shulman, one of the leading researchers in diabetes, once published an elegant experiment demonstrating the necessity of fat:
When he surgically implanted fat tissue into insulin-resistant mice, thereby making them more fat, he found that their metabolic dysfunction was cured almost instantly.
Think of fat as acting like a kind of metabolic buffer zone, absorbing excess energy and storing it safely until it is needed.
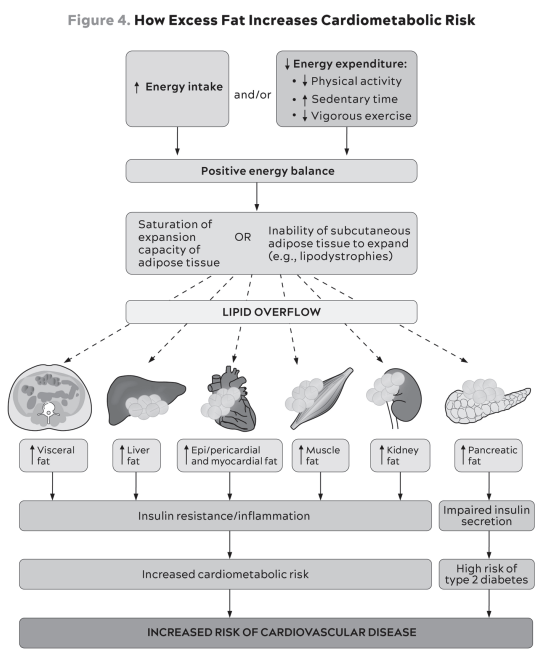 As more calories flood into your subcutaneous fat tissue, it eventually reaches
capacity and the surplus begins spilling over into other areas of your body:
into your blood, as excess triglycerides; into your liver, contributing to
NAFLD; into your muscle tissue, contributing directly to insulin resistance in
the muscle (as we’ll see); and even around your heart and your pancreas --
Source: Tchernof and Després (2013).
As more calories flood into your subcutaneous fat tissue, it eventually reaches
capacity and the surplus begins spilling over into other areas of your body:
into your blood, as excess triglycerides; into your liver, contributing to
NAFLD; into your muscle tissue, contributing directly to insulin resistance in
the muscle (as we’ll see); and even around your heart and your pancreas --
Source: Tchernof and Després (2013).
Fat also begins to infiltrate your abdomen, accumulating in between your organs.
Where subcutaneous fat is thought to be relatively harmless, this "visceral fat" is anything but.
These fat cells secrete inflammatory cytokines such as TNF-alpha and IL-6, key markers and drivers of inflammation, in close proximity to your most important bodily organs.
Fat storage capacity varies widely among individuals.
Individual fat-storage capacity seems to be influenced by genetic factors.
There are other factors at play here as well, but this explains in part why some people can be obese but metabolically healthy, while others can appear "skinny" while still walking around with three or more markers of metabolic syndrome.
If you have 20 percent body fat, making you more or less average (50th percentile) for your age and sex, that means you are carrying 40 pounds of fat throughout your body. Even if just 4.5 pounds of that is visceral fat, you would be considered at exceptionally high risk for cardiovascular disease and type 2 diabetes,
If a person is not physically active, and they are not consuming energy via their muscles, then this fat-spillover-driven insulin resistance develops much more quickly.
There are many other hormones involved in the production and distribution of fat, including testosterone, estrogen, hormone-sensitive lipase and cortisol.
Cortisol is especially potent, with a double-edged effect of depleting subcutaneous fat (which is generally beneficial) and replacing it with more harmful visceral fat.
Stress levels and sleep, both of which affect cortisol release, are pertinent to metabolism.
But insulin seems to be the most potent as far as promoting fat accumulation because it acts as kind of a one-way gate, allowing fat to enter the cell while impairing the release of energy from fat cells (via a process called lipolysis).
Like cancer, Alzheimer’s, and heart disease, type 2 diabetes is known as a "disease of civilization," meaning it has only come to prominence in the modern era.
As type 2 diabetes emerged, beginning in the early 1700s, it was at first largely a disease of the superelite, popes and artists and wealthy merchants and nobles who could afford this newly fashionable luxury food known as sugar.
In 1940 the famed diabetologist Elliott Joslin estimated that about one person in every three to four hundred was diabetic,
By 1970, around the time I was born, its prevalence was up to one in every fifty people.
Today over 11 percent of the US adult population, one in nine, has clinical type 2 diabetes,
Another 38 percent of US adults -- more than one in three -- meet at least one of the criteria for prediabetes.
When we metabolize fructose, along with certain other types of foods, it produces large amounts of uric acid, which is best known as a cause of gout
Other mammals, and even some other primates, possess an enzyme called uricase, which helps them clear uric acid. But we humans lack this important and apparently beneficial enzyme,
It is very difficult to get fat from eating too many apples, for example, because the fructose in the apple enters our system relatively slowly, mixed with fiber and water, and our gut and our metabolism can handle it normally.
But if we are drinking quarts of apple juice, it’s a different story,
Foods high in chemicals called purines, such as certain meats, cheeses, anchovies, and beer, also generate uric acid.
When a brain cell, muscle cell, gut cell, or any other type of cell breaks down glucose, it will almost instantly have more ATP (adenosine triphosphate), the cellular energy "currency," at its disposal.
The cell must expend a small amount of ATP in order to make more ATP, in the same way that you sometimes have to spend money to make money.
In glucose metabolism, this energy expenditure is regulated by a specific enzyme that prevents the cell from "spending" too much of its ATP on metabolism.
But when we metabolize fructose in large quantities, a different enzyme takes over, and this enzyme does not put the brakes on ATP "spending."
Instead, energy (ATP) levels inside the cell drop rapidly and dramatically. This rapid drop in energy levels makes the cell think that we are still hungry.
The bottom line is that even though it is rich in energy, fructose basically tricks our metabolism into thinking that we are depleting energy -- and need to take in still more food and store more energy as fat.
In my patients, I monitor several biomarkers related to metabolism, keeping a watchful eye for things like
- elevated uric acid,
- elevated homocysteine,
- chronic inflammation,
- and even mildly elevated ALT liver enzymes.
I watch the ratio of triglycerides to HDL cholesterol (it should be less than 2:1 or better yet, less than 1:1), as well as levels of VLDL, a lipoprotein that carries triglycerides
The first thing I look for, the canary in the coal mine of metabolic disorder, is elevated insulin.
One test that I like to give patients is the oral glucose tolerance test, or OGTT, where the patient swallows ten ounces of a sickly-sweet, almost undrinkable beverage called Glucola that contains seventy-five grams of pure glucose, or about twice as much sugar as in a regular Coca-Cola.
Studies have found that insulin resistance itself is associated with huge increases in one’s risk of
- cancer (up to twelvefold),
- Alzheimer’s disease (fivefold),
- and death from cardiovascular disease (almost sixfold)
CHAPTER 7 The Ticker Confronting -- and Preventing -- Heart Disease, the Deadliest Killer on the Planet
There is some risk involved in action, there always is. But there is far
more risk in failure to act. -- Harry S. Truman
While heart disease is the most prevalent age-related condition, it is also more easily prevented than either cancer or Alzheimer’s disease.
Vascular network is equally miraculous, a web of veins, arteries, and capillaries that, if stretched out and laid end to end, would wrap around the earth more than twice (about sixty thousand miles,
Cholesterol is essential to life. It is required to produce some of the most important structures in the body, including cell membranes; hormones such as testosterone, progesterone, estrogen, and cortisol; and bile acids, which are necessary for digesting
All cells can synthesize their own cholesterol, but some 20 percent of our body’s (large) supply is found in the liver, which acts as a sort of cholesterol repository, shipping it out to cells that need it and receiving it back
Because cholesterol belongs to the lipid family (that is, fats), it is not water soluble and thus cannot dissolve in our plasma
It must be carted around in tiny spherical particles called lipoproteins -- the final "L" in LDL and HDL -- which act like little cargo submarines.
Lipoproteins are part lipid (inside) and part protein (outside); the protein is essentially the vessel that allows them to travel in our plasma while carrying their water-insoluble cargo of lipids, including cholesterol, triglycerides, and phospholipids, plus vitamins and other proteins
LDLs carry more lipids, while HDLs carry more protein in relation to fat, and are therefore more dense.
Each lipoprotein particle is enwrapped by one or more large molecules, called apolipoproteins, that provide structure, stability, and, most importantly solubility to the particle.
HDL particles are wrapped in a type of molecule called apolipoprotein A (or apoA), while LDL is encased in apolipoprotein B (or apoB).
Every single lipoprotein that contributes to atherosclerosis -- not only LDL but several others carries this apoB protein signature.
Reams of research papers showing that dietary cholesterol (and particularly egg consumption) may not have much to do with heart disease at all.
Most of the actual cholesterol that we consume in our food ends up being excreted out our backsides.
The vast majority of the cholesterol in our circulation is actually produced by our own cells.
Fully half of all major adverse cardiovascular events in men (and a third of those in women), such as heart attack, stroke, or any procedure involving a stent or a graft, occur before the age of sixty-five.
Particles tagged with apoA (HDL) can cross the endothelial barrier easily in both directions,
LDL particles and other particles with the apoB protein are far more prone to getting stuck inside.
If you take a healthy coronary artery and expose it to high enough concentrations of apoB particles, over a long enough time, a certain amount of LDL (and VLDL) will get stuck in that subendothelial space and become oxidized, which then leads to it sticking together in clumps or aggregates.
In response to this incursion, the endothelium dials up the biochemical equivalent of 911, summoning specialized immune cells called monocytes
Monocytes are large white blood cells that enter the subendothelial space and transform into macrophages, larger and hungrier immune cells
The macrophage, whose name means "big eater," swallows up the aggregated or oxidized LDL, trying to remove it from the artery wall.
But if it consumes too much cholesterol, then it blows up into a foam cell,
When enough foam cells gather together, they form a "fatty streak" -- literally a streak of fat that you can see with your naked eye during an autopsy
If an HDL particle arrives at our crime scene, with the foam cells and fatty streaks, it can suck the cholesterol back out of the macrophages in a process called delipidation.
Newer research suggests that HDL has multiple other atheroprotective functions that include helping maintain the integrity of the endothelium, lowering inflammation, and neutralizing or stopping the oxidation of LDL,
The ever-growing number of foam cells begin to sort of ooze together into a mass of lipids,
This is what becomes the core of our atherosclerotic plaque.
None of what’s gone on so far is easily detectable in the various tests we typically use to assess cardiovascular risk in patients.
At a certain point in this process, the plaque may start to become calcified.
This is what (finally) shows up on a regular calcium scan.
The endothelial barrier, in particular, is uniquely vulnerable to damage from inflammation.
Evidence has piled up pointing to apoB as far more predictive of cardiovascular disease than simply LDL-C, the standard "bad cholesterol" measure.
All my patients tested for apoB regularly, and you should ask for the same test the next time you see your doctor.
Three of the major prerequisites for heart disease:
- significant lipoprotein burden or apoB,
- LDL oxidation or modification (leading to the plaques that my calcium scan revealed),
- and a high level of background inflammation.
None of these is enough to guarantee that someone will develop heart disease, but all three are necessary to develop it.
We are fortunate that many of these conditions can be modulated or nearly eliminated -- including apoB, by the way -- via lifestyle changes and medications.
Lp(a) (pronounced "el-pee-little-A"). This hot mess of a lipoprotein is formed when a garden-variety LDL particle is fused with another, rarer type of protein called apolipoprotein(a), or apo(a) for short
When a patient comes to me and says their father or grandfather or aunt, or all three, died of "premature" heart disease, elevated Lp(a) is the first thing I look for.
You should definitely ask for an Lp(a) test.
With elevated Lp(a). It does not seem to respond to behavioral interventions such as exercise and dietary changes the way that, say, LDL-C does.
How to Reduce Cardiovascular Risk
Our stories illustrate three blind spots of Medicine 2.0 when it comes to dealing with atherosclerotic disease:
- first, an overly simplistic view of lipids that fails to understand the importance of total lipoprotein burden (apoB) and how much one needs to reduce it in order to truly reduce risk;
- second, a general lack of knowledge about other bad actors such as Lp(a);
- third, a failure to fully grasp the lengthy time course of atherosclerotic disease, and the implications this carries if we seek true prevention.
When I look at a patient’s blood panel for the first time, my eyes immediately dart to two numbers: apoB and Lp(a).
I look at the other numbers, too, but these two tell me the most when it comes to predicting their risk of ASCVD.
"Atherosclerosis probably would not occur [emphasis mine] in the absence of LDL-C concentrations in excess of physiological needs (on the order of 10 to 20 mg/dL)."
Smoking and high blood pressure both damage the endothelium directly.
Smoking cessation and blood pressure control are thus non-negotiable first steps in reducing cardiovascular risk.
Monounsaturated fats, found in high quantities in extra virgin olive oil, macadamia nuts, and avocados (among other foods), do not have this effect, so I tend to push my patients to consume more of these, up to about 60 percent of total fat intake.
Typically our first line of defense (or attack), statins inhibit cholesterol synthesis, prompting the liver to increase the expression of LDLR, taking more LDL out of circulation.
They may have other benefits too, including an apparent anti-inflammatory effect,
Not everyone can take statins comfortably; about 5 percent of patients experience deal-breaking side effects, most notably statin-related muscle pain.
Most physicians and cardiology experts would still insist that one’s thirties are too young to begin to focus on primary prevention of cardiac disease.
This viewpoint is directly challenged by a 2018 JAMA Cardiology paper coauthored by Allan Sniderman, comparing ten-year versus thirty-year risk horizons in terms of prevention.
Brief Overview of Lipid-Lowering Medications
While there are seven statins on the market, I tend to start with rosuvastatin (Crestor) and only pivot from that if there is some negative effect
For people who can’t tolerate statins, I like to use a newer drug, called bempedoic acid (Nexletol), which manipulates a different pathway
It does not cause the side effects associated with statins, especially muscle soreness.
Another drug called ezetimibe (Zetia) blocks absorption of cholesterol in the GI tract. That in turn depletes the amount of cholesterol in the liver, leading once again to increased LDLR expression and greater clearance of apoB particles,
Ezetimibe pairs very well with statins because statins, which block cholesterol synthesis, tend to cause the body to reflexively increase cholesterol reabsorption in the gut -- exactly
LDL receptors can be upregulated by a class of drugs that we mentioned earlier, called PCSK9 inhibitors, which attack a protein called PCSK9 that degrades LDL receptors.
This increases the receptors’ half-life, thus improving the liver’s ability to clear apoB.
Their most common use is in addition to statins;
Alas, statins do not reduce Lp(a), but PCSK9 inhibitors do in most patients, typically to the tune of about 30 percent.
In cases where nutritional changes are insufficient, and in cases where genetics render dietary interventions useless, fibrates are the drug of choice.
Ethyl eicosapentaenoic acid (Vascepa), a drug derived from fish oil and consisting of four grams of pharmaceutical-grade eicosapentaenoic acid (EPA), also has FDA approval to reduce LDL in patients with elevated triglycerides.
CHAPTER 8 The Runaway Cell New Ways to Address the Killer That Is Cancer
You may have to fight a battle more than once to win it. -- Margaret
Thatcher
In 2017 there were more cancer deaths among people between forty-five and sixty-four than from heart disease, liver disease, and stroke combined.
What Is Cancer?
Cancer cells are different from normal cells in two important ways.
Contrary to popular belief, cancer cells don’t grow faster than their noncancerous counterparts; they just don’t stop growing when they are supposed to.
This process is thought to begin when normal cells acquire certain genetic mutations. For example, a gene called PTEN, which normally stops cells from growing or dividing (and eventually becoming tumors), is often mutated or "lost" in people with cancer,
The second property that defines cancer cells is their ability to travel from one part of the body to a distant site where they should not be. This is called metastasis,
This spreading is what turns a cancer from a local, manageable problem to a fatal, systemic disease.
One of the biggest obstacles to a "cure" is the fact that cancer is not one single, simple, straightforward disease, but a condition with mind-boggling complexity.
About two decades ago, the National Cancer Institute launched a huge and ambitious study called The Cancer Genome Atlas, whose goal was to sequence cancer tumor cells
Rather than uncovering a definite pattern of genetic changes driving each type of cancer, the study found enormous complexity.
A handful of genes emerged as drivers, including TP53 (also known as p53, found in half of all cancers), KRAS (common in pancreatic cancer), PIC3A (common in breast cancer), and BRAF (common in melanoma), but very few if any of these well-known mutations were shared across all tumors.
In fact, there didn’t seem to be any individual genes that "caused" cancer at all; instead, it seemed to be random somatic mutations that combined to cause cancers.
If two women have breast cancer, at the same stage, their tumor genomes are likely to be very different from each other.
In 2011, two leading cancer researchers named Douglas Hanahan and Robert Weinberg identified two key hallmarks of cancer that may lead -- and in fact have led -- to new treatments, as well as potential methods of reducing cancer risk.
- The first such hallmark is the fact that many cancer cells have an altered metabolism, consuming huge amounts of glucose.
- Second, cancer cells seem to have an uncanny ability to evade the immune system,
Cancer Metabolism
We tend to think of cancer as primarily a genetic disease, driven by mutations of unknown cause.
In the 1920s, a German physiologist named Otto Warburg discovered that cancer cells had a strangely gluttonous appetite for glucose, devouring it at up to forty times the rate of healthy tissues.
But these cancer cells weren’t "respiring" the way normal cells do, consuming oxygen and producing lots of ATP, the energy currency of the cell, via the mitochondria.
Areas with abnormally high glucose concentrations indicate the possible presence of a tumor.
Normal aerobic cellular respiration produces only energy, in the form of ATP, plus water and carbon dioxide, which aren’t much use as building materials (also, we exhale the latter two).
The Warburg effect, also known as anaerobic glycolysis, turns the same amount of glucose into a little bit of energy and a whole lot of chemical building blocks -- which are then used to build new cells rapidly.
The American Cancer Society reports that excess weight is a leading risk factor for both cancer cases and deaths, second only to smoking.
Globally, about 12 to 13 percent of all cancer cases are thought to be attributable to obesity.
Type 2 diabetes also increases the risk of certain cancers, by as much as double in some cases (such as pancreatic and endometrial cancers).
And extreme obesity (BMI ≥ 40) is associated with a 52 percent greater risk of death from all cancers in men, and 62 percent in women.
There is already some evidence that tinkering with metabolism can affect cancer rates.
Laboratory animals on calorically restricted (CR) diets tend to die from cancer at far lower rates than control animals on an ad libitum (all-they-can-eat) diet.
I’m not suggesting that it’s possible to "starve" cancer or that any particular diet will magically make cancer go away; cancer cells always seem to be able to obtain the energy supply they need.
What I am saying is that we don’t want to be anywhere on that spectrum of insulin resistance to type 2 diabetes, where our cancer risk is clearly elevated.
New Treatments
Published in Nature in 2018, with Mukherjee and Cantley as senior authors, the study found that a combination of a ketogenic diet and PI3K inhibitors improved the responses to treatment of mice that had been implanted with human cancer tumors.
Work by Valter Longo of the University of Southern California and others has found that fasting, or a fasting-like diet, increases the ability of normal cells to resist chemotherapy, while rendering cancer cells more vulnerable to the treatment.
The Promise of Immunotherapy
The immune system is programmed to distinguish "nonself" from "self" -- that is, to recognize invading pathogens and foreign bodies among our own healthy native cells, and then to kill or neutralize the harmful agents.
While cancer cells are abnormal and dangerous, they are technically still our cells
So for a cancer immunotherapy to succeed, we essentially need to teach the immune system to recognize and kill our own cells that have turned cancerous.
Only 8 percent of potential cancer deaths could be prevented by immunotherapy,
Early Detection
The evidence is overwhelming that catching cancer early is almost always net beneficial.
The problem is that we’re still not very good at detecting cancer in these early stages -- yet.
Low-dose CT scans for lung cancer.
These scans are currently recommended in smokers and former smokers,
One newer technique that can enhance the ability of a screening MRI to differentiate between a cancer and noncancer is something called diffusion-weighted imaging with background subtraction, or DWI for short.
The Grail test, known as Galleri, looks at methylation patterns of the cell-free DNA, which are basically chemical changes to the DNA molecules that suggest the presence of cancer.
Galleri test proved to have a very high specificity, about 99.5 percent,
The trade-off is that the resulting sensitivity can be low, depending on the stage.
The thing to keep in mind here, however, is that this test still has much higher resolution than radiographic tests such as MRI or mammogram.
If the first rule of cancer is "Don’t get cancer," the second rule is "Catch it as soon as possible."
CHAPTER 9 Chasing Memory Understanding Alzheimer’s Disease and Other Neurodegenerative Diseases
The greatest obstacle to discovery is not ignorance -- it is the illusion
of knowledge. -- Daniel J. Boorstin
A third thing that I always check is their APOE genotype, the gene related to Alzheimer’s disease risk
Alzheimer’s disease is the most common, but there are other neurodegenerative diseases that concern us.
The most prevalent of these are Lewy body dementia and Parkinson’s disease, which are actually different forms of a related disorder
Having the e4 gene variant merely signals increased risk. It’s not a done deal.
Understanding Alzheimer’s
Researchers identified the substance in the plaques as a peptide called amyloid-beta.
Amyloid-beta is a by-product that is created when a normally occurring substance called amyloid precursor protein, or APP, a membrane protein that is found in neuronal synapses, is cleaved into three pieces.
Normally, APP is split into two pieces, and everything is fine.
But when APP is cut in thirds, one of the resulting fragments then becomes "misfolded," meaning it loses its normal structure (and thus its function) and becomes chemically stickier, prone to aggregating in clumps.
Amyloid also triggers the aggregation of another protein called tau, which in turn leads to neuronal inflammation and, ultimately, brain shrinkage.
Several dozen drugs have been developed that target amyloid-beta in
But even when they succeed in clearing amyloid or slowing its production, these drugs have yet to show benefit in improving patients’ cognitive function or slowing the progression of the disease.
Every single one of them failed.
Autopsy studies have found that more than 25 percent of cognitively normal people nevertheless had large deposits of amyloid in their brains when they died -- some of them with the same degree of plaque buildup as patients who died with severe dementia.
But for some reason, these people displayed no cognitive symptoms.
More recent studies have found that the reverse can also be true: some patients with all the symptoms of Alzheimer’s disease, including significant cognitive decline, have little to no amyloid in their brains,
It appears, then, that the presence of amyloid-beta plaques may be neither necessary for the development of Alzheimer’s disease nor sufficient to cause it.
Lewy body dementia and Parkinson’s disease are associated with the accumulation of a neurotoxic protein called alpha-synuclein, which builds up in aggregates known as Lewy bodies
Can Neurodegenerative Disease Be Prevented?
A two-year randomized controlled trial in Finland, published in 2015, found that interventions around nutrition, physical activity, and cognitive training helped maintain cognitive function and prevent cognitive decline among a group of more than 1,200 at-risk older adults.
In a broader sense, all of us are at some risk of Alzheimer’s disease and other neurodegenerative disease.
Women have a greater age-adjusted risk of Alzheimer’s, as well as faster rates of disease progression overall, regardless of age and educational level.
While female Alzheimer’s patients outnumber men by two to one, the reverse holds true for Lewy body dementia and Parkinson’s, both of which are twice as prevalent in men.
Dementia has an extremely long prologue.
Its beginnings are so subtle
Noticeable memory problems such as forgetting common words and frequently losing important objects
Performance on cognitive tests begins to slip.
Subtler signs of cognitive changes often become apparent well before patients meet the criteria for MCI.
Parkinson’s may show up as subtle changes in movement patterns, a frozen facial expression, stooped posture or shuffling gait, a mild tremor, or even changes in a person’s handwriting
Early stages of Lewy body dementia may exhibit similar physical symptoms, but with slight cognitive changes as well; both may exhibit alterations in mood, such as depression or anxiety.
An important first step with any patient who may have cognitive issues is to subject them to a grueling battery of tests.
These are clinically validated, highly complex tests that cover every domain of cognition and memory, including executive function, attention, processing speed, verbal fluency and memory (recalling a list of words), logical memory (recalling a phrase in the middle of a paragraph), associative memory (linking a name to a face), spatial memory (location of items in a room), and semantic memory (how many animals you can name in a minute, for example).
Can they correctly identify scents such as coffee, for example? Olfactory neurons are among the first to be affected by Alzheimer’s disease.
One reason why Alzheimer’s and related dementias can be so tricky to diagnose is that our highly complex brains are adept at compensating for damage, in a way that conceals these early stages of neurodegeneration.
When we have a thought or a perception, it’s not just one neural network that is responsible for that insight, or that decision, but many individual networks working simultaneously
The more of these networks and subnetworks that we have built up over our lifetime, via education or experience, or by developing complex skills such as speaking a foreign language or playing a musical instrument, the more resistant to cognitive decline we will tend to be.
People with better movement patterns, and a longer history of moving their bodies, such as trained or frequent athletes, tend to resist or slow the progression of the disease as compared to sedentary people.
Exercise is the only intervention shown to delay the progression of Parkinson’s.
Alternatives to Amyloid
1968 paper that defined Alzheimer’s disease as a common age-related condition, Blessed, Tomlinson, and Roth had also noted severe vascular damage in the brains of their deceased study subjects.
In the early 1990s, a Case Western Reserve neurologist named Jack de la Torre was flying to Paris for a conference and thinking about the origins of Alzheimer’s disease.
The amyloid hypothesis was still fairly new, but it didn’t sit well with de la Torre because of what he had observed in his own lab.
The brain is a greedy organ. It makes up just 2 percent of our body weight, yet it accounts for about 20 percent of our total energy expenditure.
Its eighty-six billion neurons each have between one thousand and ten thousand synapses connecting them to other neurons or target cells,
Brain cells metabolize glucose in a different way from the rest of the body; they do not depend on insulin, instead absorbing circulating glucose directly, via transporters that essentially open a gate in the cell membrane.
If we lack new sources of glucose, the brain’s preferred fuel, the liver converts our fat into ketone bodies, as an alternative energy source that can sustain us for a very long time, depending on the extent of our fat stores.
When our fat runs out, we will begin to consume our own muscle tissue, then our other organs, and even bone, all in order to keep the brain running at all costs.
The brain is the last thing to shut off.
His "barf bag theory," as he jokingly called it, was that Alzheimer’s disease is primarily a vascular disorder of the brain.
The amyloid plaques and tangles come later, as a consequence rather than a cause.
There was already evidence to support his theory.
Alzheimer’s is more likely to be diagnosed in patients who have suffered a stroke, which typically results from a sudden blockage of blood flow in specific regions of the brain.
Additionally, it has been established that people with a history of cardiovascular disease are at a higher risk of developing Alzheimer’s disease.
Evidence also demonstrates a linear relationship between cognitive decline and increased intimal media thickness in the carotid artery,
Drop in blood flow seems to predict when a person will transition from preclinical Alzheimer’s disease to MCI, and on to full-fledged dementia.
Another compelling and perhaps parallel theory of Alzheimer’s disease says that it stems from abnormal glucose metabolism in the brain.
Having type 2 diabetes doubles or triples your risk
Chronically elevated blood glucose, as seen in type 2 diabetes and prediabetes/insulin resistance, can directly damage the vasculature of the brain.
Insulin seems to play a key role in memory function. Insulin receptors are highly concentrated in the hippocampus, the memory center of the brain.
Studies have found that spraying insulin right into subjects’ noses -- administering it as directly as possible into their brains -- quickly improves cognitive performance and memory, even in people who have already been diagnosed with Alzheimer’s disease.
One study found that intranasal insulin helped preserve brain volume in Alzheimer’s patients.
Clearly, it is helpful to get glucose into neurons; insulin resistance blocks this.
The Role of APOE e4
It is still not completely clear how or why, but e4 seems to accelerate other risk factors and driver mechanisms for Alzheimer’s -- particularly
A woman with one copy of e4 is four times more likely to develop the disease than a man
The protein for which it codes, APOE (apolipoprotein E), plays an important role in both cholesterol transport and glucose metabolism.
It serves as the main cholesterol carrier in the brain, moving cholesterol across the blood-brain barrier to supply the neurons
People with the e4 allele appear to have defects in both cholesterol transport and glucose metabolism, to a degree not seen in those with e2 or e3.
For millions of years, all our post-primate ancestors were e4/e4.
The e3 mutation showed up about 225,000 years
E2 is a relative latecomer, arriving only in the last 10,000 years.
Data from present-day populations with a high prevalence of e4 suggest that it may have been helpful for survival in environments with high levels of infectious disease:
This survival benefit may have been due to the role of APOE e4 in promoting inflammation, which can be beneficial in some situations (e.g., fighting infection) but harmful in others (e.g., modern life).
The e4 variant also seems to be maladaptive in other ways, such as in dealing with our modern diets.
Disrupting the brain’s ability to regulate insulin levels and maintain glucose homeostasis in the body.
It is now believed that Alzheimer’s risk and the effect of APOE are also powerfully dependent on other Alzheimer’s-risk-related genes that a person might carry, such as Klotho,
The Preventive Plan
Our goal is to improve glucose metabolism, inflammation, and oxidative stress.
Recommendation for someone like her would be to switch to a Mediterranean-style diet, relying on more monounsaturated fats and fewer refined carbohydrates, in addition to regular consumption of fatty fish.
There is some evidence that supplementation with the omega-3 fatty acid DHA, found in fish oil, may help maintain brain health, especially in e4/e4 carriers.
Higher doses of DHA may be required because of e4
This is also one area where a ketogenic diet may offer a real functional advantage:
When someone is in ketosis, their brain relies on a mix of ketones and glucose for fuel.
Single most powerful item in our preventive tool kit is exercise, it helps maintain glucose homeostasis, and it improves the health of our vasculature.
Focusing on steady endurance exercise to improve her mitochondrial efficiency.
This had a side benefit in that it helped manage her off-the-charts high cortisol levels, due to stress;
Endurance exercise produces factors that directly target regions of the brain responsible for cognition and memory.
It also helps lower inflammation and oxidative stress.
Strength training is likely just as important.
A study looking at nearly half a million patients in the United Kingdom found that grip strength, an excellent proxy for overall strength, was strongly and inversely associated with the incidence of dementia
I now tell patients that exercise is, full stop and hands down, the best tool we have in the neurodegeneration prevention tool kit.
Sleep is also a very powerful tool
Sleep is when our brain heals itself; while we are in deep sleep our brains are essentially "cleaning house," sweeping away intracellular waste that can build up between our neurons.
If poor sleep is accompanied by high stress and elevated cortisol levels, as in Stephanie’s case, that acts almost as a multiplier of risk, as it contributes to insulin resistance and damaging the hippocampus at the same time.
Hypercortisolemia (excess cortisol due to stress) impairs the release of melatonin, the hormone that normally signals to our brains that it is time to go to sleep
Hearing loss is clearly associated with Alzheimer’s disease, but it’s not a direct symptom.
Hearing loss may be causally linked to cognitive decline, because folks with hearing loss tend to pull back and withdraw from interactions with others.
While depression is also associated with Alzheimer’s disease, it appears to be more of a symptom than a risk factor
Treating depression in patients with MCI or early Alzheimer’s disease does appear to help reduce some other symptoms of cognitive decline.
Another surprising intervention that may help reduce systemic inflammation, and possibly Alzheimer’s disease risk, is brushing and flossing one’s teeth.
P. gingivalis that commonly causes gum disease, is responsible for large increases in levels of inflammatory markers such as IL-6.
Better oral health correlates strongly with better overall health, particularly in terms of cardiovascular disease risk,
Until about 2019 I was very skeptical of the data linking sauna use to brain and heart health.
I’m not quite as confident that regular sauna use will reduce your risk of Alzheimer’s disease as I am that exercise will do so, but I am much more confident than I was at the outset of my journey.
Literature suggests that at least four sessions per week, of at least twenty minutes per session, at 179 degrees Fahrenheit (82 degrees Celsius) or hotter seems to be the sweet spot to reduce the risk of Alzheimer’s by about 65 percent (and the risk of ASCVD by 50 percent).
Other potential interventions that have shown some promise
Lowering homocysteine with B vitamins, while optimizing omega-3 fatty acids.
Higher vitamin D levels have been correlated with better memory in e4/e4 patients
But it’s difficult to know from the current literature if this means supplementing with vitamin D will reduce risk of AD.
Hormone replacement therapy for women during the transition from perimenopause to menopause seems promising, especially for women with at least one copy of e4.
Broadly, our strategy should be based on the following principles:
WHAT’S GOOD FOR THE HEART IS GOOD FOR THE BRAIN. That is, vascular health (meaning low apoB, low inflammation, and low oxidative stress)
WHAT’S GOOD FOR THE LIVER (AND PANCREAS) IS GOOD FOR THE BRAIN. Metabolic health is crucial to brain health.
TIME IS KEY. We need to think about prevention early,
OUR MOST POWERFUL TOOL FOR PREVENTING COGNITIVE DECLINE IS EXERCISE.
PART III
CHAPTER 10 Thinking Tactically Building a Framework of Principles That Work for You
Absorb what is useful, discard what is useless, and add what is
specifically your own. -- Bruce Lee
Cancer, as well as heart disease, type 2 diabetes, and dementia (along with a few others), became collectively known as "diseases of civilization," because they seemed to have spread in lockstep with the industrialization and urbanization
Our genes no longer match our environment. Thus, we must be cunning in our tactics if we are to adapt and thrive
In Medicine 3.0, we have five tactical domains
- The first is exercise,
- I break it down into its components of aerobic efficiency, maximum aerobic output (VO2 max), strength, and stability,
- Next is diet or nutrition -- or as I prefer to call it, nutritional biochemistry.
- The third domain is sleep,
- The fourth domain encompasses a set of tools and techniques to manage and improve emotional health.
- Our fifth and final domain consists of the various drugs, supplements, and hormones. I lump these into one bucket called exogenous molecules, meaning molecules we ingest that come from outside the body.
When I evaluate new patients, I’m always asking three key questions:
- Are they overnourished or undernourished?
- Are they undermuscled or adequately muscled?
- Are they metabolically healthy or not?
I used to recommend long periods of water-only fasting for some of my patients -- and practiced it myself. But I no longer do so, because I’ve become convinced that the drawbacks (mostly having to do with muscle loss and undernourishment) outweigh its metabolic benefits in all but my most overnourished patients.
CHAPTER 11 Exercise The Most Powerful Longevity Drug
I never won a fight in the ring; I always won in preparation. -- Muhammad
Ali
Reams of data supporting the notion that even a fairly minimal amount of exercise can lengthen your life by several years.
If exercise is not a part of your life at the moment, you are not alone -- 77 percent of the US population is like you.
Going from zero weekly exercise to just ninety minutes per week can reduce your risk of dying from all causes by 14 percent.
Peak aerobic cardiorespiratory fitness, measured in terms of VO2 max, is perhaps the single most powerful marker for longevity.
At rest, someone my size might require about 300 ml of oxygen per minute in order to generate enough ATP, but if I go outside and jog around my neighborhood, the energy demands ramp up.
At this level of intensity, someone my size might require 2,500 to 3,000 ml of oxygen per minute, an eight- to tenfold increase from when I was sitting on the couch.
Eventually, I will reach the point at which I just can’t produce any more energy via oxygen-dependent pathways,
The amount of oxygen that I am using at this level of effort represents my VO2 max.
An average forty-five-year-old man will have a VO2 max around 40 ml/kg/min, while an elite endurance athlete will likely score in the high 60s and above.
An unfit person in their thirties or forties, on the other hand, might score only in the high 20s on a VO2 max test,
A 2018 study in JAMA that followed more than 120,000 people found that higher VO2 max (measured via a treadmill test) was associated with lower mortality across the board.
A person who smokes has a 40 percent greater risk of all-cause mortality
This study found that someone of below-average VO2 max for their age and sex (that is, between the 25th and 50th percentiles) is at double the risk of all-cause mortality compared to someone in the top quartile
Thus, poor cardiorespiratory fitness carries a greater relative risk of death than smoking.
Someone in the bottom quartile of VO2 max for their age group (i.e., the least fit 25 percent) is nearly four times likelier to die than someone in the top quartile -- and five times likelier to die than a person with elite-level (top 2.3 percent) VO2 max.
Even just climbing from the bottom 25 percent into the 25th to 50th percentile (e.g., least fit to below average) means you have cut your risk of death nearly in half,
"Being unfit carried a greater risk than any of the cardiac risk factors examined," the authors concluded.
muscle may be almost as powerfully correlated with living longer.
A ten-year observational study of roughly 4,500 subjects ages fifty and older found that those with low muscle mass were at 40 to 50 percent greater risk of mortality than controls,
It’s not the mere muscle mass that matters but the strength of those muscles,
Strength may even trump cardiorespiratory fitness, at least one study suggests.
Researchers following a group of approximately 1,500 men over forty with hypertension, for an average of about eighteen years, found that even if a man was in the bottom half of cardiorespiratory fitness, his risk of all-cause mortality was still almost 48 percent lower if he was in the top third of the group in terms of strength versus the bottom third.
He found that in numerous randomized clinical trials, exercise-based interventions performed as well as or better than multiple classes of pharmaceutical drugs at reducing mortality from coronary heart disease, prediabetes or diabetes, and stroke.
Exercise really does act like a drug. To be more precise, it prompts the body to produce its own, endogenous drug-like chemicals.
When we are exercising, our muscles generate molecules known as cytokines that send signals to other parts of our bodies, helping to strengthen our immune system and stimulate the growth of new muscle and stronger bones.
Endurance exercise such as running or cycling helps generate another potent molecule called brain-derived neurotrophic factor, or BDNF, that improves the health and function of the hippocampus,
Longitudinal and cross-sectional studies find that fat-free mass (meaning mostly muscle mass) and activity levels remain relatively consistent as people age from their twenties and thirties into middle age.
But both physical activity levels and muscle mass decline steeply after about age sixty-five, and then even more steeply after about seventy-five.
It’s as if people just fall off a cliff sometime in their mid-seventies.
By age eighty, the average person will have lost eight kilograms of muscle, or about eighteen pounds, from their peak.
But people who maintain higher activity levels lose much less muscle, more like three to four kilograms on average.
Seniors with the least muscle mass (also known as lean mass) are at the greatest risk of dying from all causes.
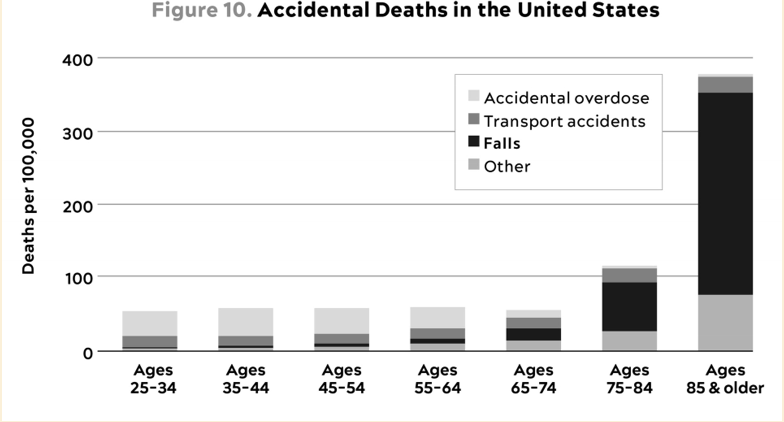 Falls are by far the leading cause of accidental deaths in those ages
sixty-five and older—and this is without even counting the people who die three
or six or twelve months after their nonfatal but still serious fall pushed them
into a long and painful decline. Eight hundred thousand older people are
hospitalized for falls each year according to the CDC. -- Source: CDC (2021).
Falls are by far the leading cause of accidental deaths in those ages
sixty-five and older—and this is without even counting the people who die three
or six or twelve months after their nonfatal but still serious fall pushed them
into a long and painful decline. Eight hundred thousand older people are
hospitalized for falls each year according to the CDC. -- Source: CDC (2021).
Eight hundred thousand older people are hospitalized for falls each year, according to the CDC.
I decided: each of us needs to be training for the Centenarian Decathlon.
The Centenarian Decathlon
Think of the Centenarian Decathlon as the ten most important physical tasks you will want to be able to do for the rest of your life.
I start by presenting my patients with a long list of physical tasks that might include some of the following:
- Hike 1.5 miles on a hilly trail.
- Get up off the floor under your own power, using a maximum of one arm for support.
- Pick up a young child from the floor.
- Carry two five-pound bags of groceries for five blocks.
- Lift a twenty-pound suitcase into the overhead compartment of a plane.
- Balance on one leg for thirty seconds, eyes open. (Bonus points: eyes closed, fifteen seconds.)
- Have sex.
- Climb four flights of stairs in three minutes.
- Open a jar.
- Do thirty consecutive jump-rope skips.
Let’s say the kid weighs twenty-five or thirty pounds. That’s basically the same as doing a squat while holding a thirty-pound dumbbell in front of you
Your muscle strength will decline by about 8 to 17 percent per decade -- accelerating as time goes on.
If you want to pick up that thirty-pound grandkid or great-grandkid when you’re eighty, you’re going to have to be able to lift about fifty to fifty-five pounds now.
In every case, you need to be doing much more now, to armor yourself against the natural and precipitous decline in strength and aerobic capacity that you will undergo as you
I would probably add in some of the following events:
- Swim half a mile in twenty minutes.
- Walk with a thirty-pound dumbbell in each hand for one minute.
- Draw back and fire a fifty-pound compound bow.
- Do five pull-ups.
- Climb ninety steps in two minutes (VO2 max = 32).
- Dead-hang for one minute.
- Drive a race car within 5 to 8 percent of the pace I can do so today.
- Hike with a twenty-pound backpack for an hour.
- Carry my own luggage.
- Walk up a steep hill.
We need to abolish that decrepit stereotype and create a new narrative -- perhaps it’s not about being great at any one pursuit, but about being pretty good at just about everything.
CHAPTER 12 Training 101 How to Prepare for the Centenarian Decathlon
It is impossible to produce superior performance unless you do something
different from the majority. -- Sir John Templeton
The three dimensions in which we want to optimize our fitness are aerobic endurance and efficiency (aka cardio), strength, and stability.
We are interested in two particular regions of this continuum:
- long, steady endurance work, such as jogging or cycling or swimming, where we are training in what physiologists call zone 2,
- and maximal aerobic efforts, where VO2 max comes into play.
The strength side of the equation seems simpler, at first: if you use your muscles to counter some resistance, they will adapt and grow stronger.
It’s equally important that we avoid injury in the process. This is where stability comes in.
It’s a bit hard to define, but I think of stability as the solid foundation that enables us to do everything else that we do, without getting injured.
Aerobic Efficiency: Zone 2
Primary benefit, is that it "burns calories." And it does, but we are more interested in a finer distinction -- not calories, but fuels.
How we utilize different fuels, glucose and fatty acids, is critical
Mitochondria, those tiny little intracellular organelles that produce much of our energy.
These cellular "engines" can burn both glucose and fat,
Healthy mitochondria are also important to maintaining the health of our brain, and to controlling potential bad actors like oxidative stress and inflammation.
Zone 2 is more or less the same in all training models: going at a speed slow enough that one can still maintain a conversation but fast enough that the conversation might be a little strained.
While glucose can be metabolized in multiple different ways, fatty acids can be converted to energy only in the mitochondria.
Typically, someone working at a lower relative intensity will be burning more fat, while at higher intensities they would rely more on glucose.
The healthier and more efficient your mitochondria, the greater your ability to utilize fat, which is by far the body’s most efficient and abundant fuel source.
San Millán’s insight was that the sedentary subjects needed to be training in a manner similar to the Tour de France–bound cyclists he worked with.
A professional cyclist might spend thirty to thirty-five hours a week training on his or her bike, and 80 percent of that time in zone 2.
(The catch is that a professional rider’s zone 2 output feels like zone 5 for most people.)
When we are exercising in zone 2, most of the work is being done by our type 1, or "slow-twitch," muscle fibers.
These are extremely dense with mitochondria
If we pick up the pace, we begin to recruit more type 2 ("fast-twitch") muscle fibers, generate more lactate in the process,
In technical terms, San Millán describes zone 2 as the maximum level of effort that we can maintain without accumulating lactate.
The more efficient our mitochondrial "engine," the more rapidly we can clear lactate,
I often test my own lactate while I am working out this way, using a small handheld lactate monitor,
The goal is to keep lactate levels constant, ideally between 1.7 and 2.0 millimoles.
If you know your maximum heart rate -- not estimated, but your actual maximum, the highest number you’ve ever seen on a heart rate monitor -- your zone 2 will correspond to between approximately 70 and 85 percent of that peak
"talk test." If you’re at the top of zone 2, you should be able to talk but not particularly interested in holding a conversation. If you can’t speak in complete sentences at all, you’re likely into zone 3,
If you can comfortably converse, you’re likely in zone 1,
In San Millán and Brooks’s study, the professional cyclists produced about three hundred watts of power in zone 2, while the sedentary, metabolically unhealthy subjects could generate only about one hundred watts at the same relative level of intensity.
People with obesity or other metabolic problems will tend to have much higher resting lactate levels, a clear sign that their mitochondria are not functioning optimally,
This means that they are relying almost totally on glucose (or glycogen) for all their energy needs -- and
It seems unjust, but the people who most need to burn their fat, the people with the most of it, are unable to unlock virtually any of that fat to use as energy,
When we do aerobic exercise, it stimulates the creation of many new and more efficient mitochondria through a process called mitochondrial biogenesis, while eliminating ones that have become dysfunctional via a recycling process called mitophagy
about three hours per week of zone 2, or four 45-minute sessions, is the minimum required for most people
Side benefit of zone 2 is that it also helps with cognition, by increasing cerebral blood flow and by stimulating the production of BDNF, brain-derived neurotrophic factor,
Maximum Aerobic Output: VO2 Max
This is a much higher level of intensity -- a hard, minutes-long effort, but still well short of an all-out sprint.
At VO2 max, we are using a combination of aerobic and anaerobic pathways to produce energy,
But we are at our maximum rate of oxygen consumption. Oxygen consumption is the key.
Typically, for patients who are new to exercising, we introduce VO2 max training after about five or six months of steady zone 2 work.
It’s striking how steeply VO2 max declines with age, and how this decline corresponds to diminished functional capacity.
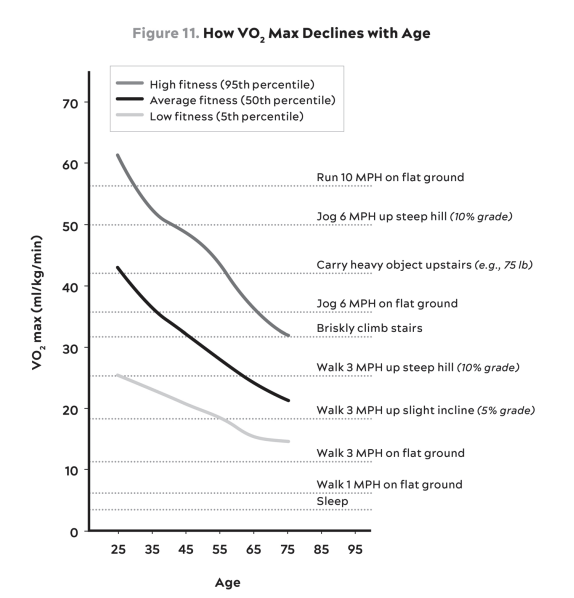 Source: Graph by Jayson Gifford, Brigham Young University, based on data from
Ligouri (2020).
Source: Graph by Jayson Gifford, Brigham Young University, based on data from
Ligouri (2020).
Ideally, I want them to target the "elite" range for their age and sex (roughly the top 2 percent).
Studies suggest that your VO2 max will decline by roughly 10 percent per decade -- and up to 15 percent per decade after the age of fifty.
Improving your VO2 max from the very bottom quartile to the quartile above (i.e., below average) is associated with almost a 50 percent reduction in all-cause mortality,
Longer and more focused training can yield much larger gains over extended periods of time -- periods measured in years, not weeks.
One study found that boosting elderly subjects’ VO2 max by 6 ml/kg/min, or about 25 percent, was equivalent to subtracting twelve years from their age.
The tried-and-true formula for these intervals is to go four minutes at the maximum pace you can sustain for this amount of time.
Then ride or jog four minutes easy, which should be enough time for your heart rate to come back down to below about one hundred beats per minute.
Repeat this four to six times and cool down.
a single workout per week in this zone will generally suffice.
You want to make sure that you get as close to fully recovered as possible before beginning the next set.
If you fail to recover sufficiently between sets, you will not be able to reach your peak effort in the working sets
The kind of aerobic fitness that most people actually need in the course of their lives, it basically boils down to being really good at going slow for a long time, but also able to go hard and fast when needed.
Strength
An eighty-year-old man will have about 40 percent less muscle tissue (as measured by cross section of the vastus lateralis, aka the "quad" muscle of the thigh) than he did at twenty-five.
We lose muscle strength about two to three times more quickly than we lose muscle mass.
The biggest single change in the aging muscle is the atrophy of our fast twitch or type 2 muscle fibers.
In its most extreme form, this muscle loss is called sarcopenia,
Sarcopenia is a prime marker for a broader clinical condition called frailty,
Where a person meets three of these five criteria: unintended weight loss; exhaustion or low energy; low physical activity; slowness in walking; and weak grip strength
It is very difficult to put on muscle mass later in life.
We measure BMD in every patient, every year, looking at both of their hips and their lumbar spine using DEXA. This also measures body fat and lean mass,
Bone density diminishes on a parallel trajectory to muscle mass, peaking as early as our late twenties before beginning a slow, steady decline.
For women, this decline happens much more quickly once they hit menopause, if they are not on HRT
(yet another reason we heavily favor HRT),
Because estrogen is essential for bone strength -- in both men and women.
Other risk factors for low bone density include
- genetics (family history),
- history of smoking, long use of corticosteroids (e.g., for asthma or autoimmune conditions),
- drugs that block estrogen (e.g., women taking such drugs for breast cancer),
- low muscle mass
- and being undernourished.
Up to one-third of people over sixty-five who fracture their hip are dead within a year.
When we detect low or rapidly declining BMD in a middle-aged person, we use the following four strategies:
- Optimize nutrition, focusing on protein and total energy needs
- Heavy loading-bearing activity. Strength training, especially with heavy weights
- HRT, if indicated.
- Drugs to increase BMD, if indicated.
I’m less concerned with how big my biceps are or how much I can bench press. A far more important measure of strength, I’ve concluded, is how much heavy stuff you can carry.
I’ve also become semiobsessed with an activity called rucking,
(A good goal is to be able to carry one-quarter to one-third of your body weight once you develop enough strength and stamina.
Fundamentally I structure my training around exercises that improve the following:
- Grip strength, how hard you can grip with your hands, which involves everything from your hands to your lats
- Attention to both concentric and eccentric loading for all movements,
- Rucking down hills is a great way to work on eccentric strength, because it forces you to put on the "brakes."
- Pulling motions, at all angles from overhead to in front of you, which also requires grip strength (e.g., pull-ups and rows).
- Hip-hinging movements, such as the deadlift and squat, but also step-ups, hip-thrusters, and countless single-leg variants of exercises that strengthen the legs, glutes, and lower back.
Many studies suggest that grip strength -- literally, how hard you can squeeze something with one hand -- predicts how long you are likely to live, while low grip strength in the elderly is considered to be a symptom of sarcopenia,
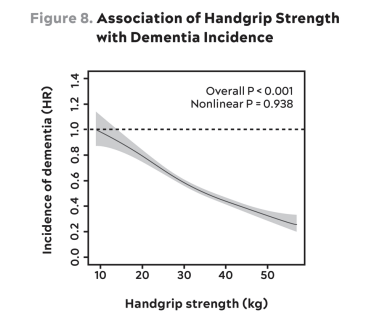 The incidence of dementia declines with increasing handgrip strength. Note that
data are presented as hazard ratios in comparison with the weakest group (e.g.,
0.4 = 40 percent reduction in risk). Thus, someone with 40 kg grip strength has
about 40 percent as much risk of dementia as someone with 10 kg. -- Source:
Esteban-Cornejo et al. (2022)
The incidence of dementia declines with increasing handgrip strength. Note that
data are presented as hazard ratios in comparison with the weakest group (e.g.,
0.4 = 40 percent reduction in risk). Thus, someone with 40 kg grip strength has
about 40 percent as much risk of dementia as someone with 10 kg. -- Source:
Esteban-Cornejo et al. (2022)
Training grip strength is not overly complicated. One of my favorite ways to do it is the classic farmer’s carry,
One of the standards we ask of our male patients is that they can carry half their body weight in each hand (so full body weight in total) for at least one minute, and for our female patients we push for 75 percent of that weight.
Another way to test your grip is by dead-hanging from a pull-up bar for as long as you can.
Here we like to see men hang for at least two minutes and women for at least ninety seconds at the age of forty.
One of the tests we have our patients perform is stepping onto and off an eighteen-inch block and taking three full seconds to reach the ground
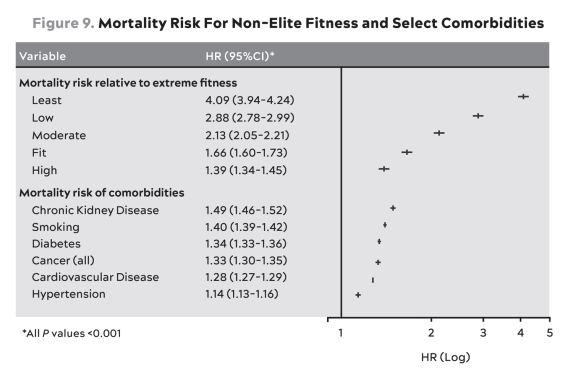 This table expresses all-cause mortality risk for different fitness levels
compared to individuals in the top 2% of VO2 max for their age and sex
(“extreme fitness”) [TOP] and for various comorbidities—that is, people with
versus without each illness. [BOTTOM] Fitness groups are divided by percentile:
Least (<20th percentile); Low (21st to 40th percentile); Moderate (41st to 60th
percentile); Fit (61st to 80th percentile); High (81st to 97th percentile). --
Source: Kokkinos et al. (2022).
This table expresses all-cause mortality risk for different fitness levels
compared to individuals in the top 2% of VO2 max for their age and sex
(“extreme fitness”) [TOP] and for various comorbidities—that is, people with
versus without each illness. [BOTTOM] Fitness groups are divided by percentile:
Least (<20th percentile); Low (21st to 40th percentile); Moderate (41st to 60th
percentile); Fit (61st to 80th percentile); High (81st to 97th percentile). --
Source: Kokkinos et al. (2022).
CHAPTER 13 The Gospel of Stability Relearning How to Move to Prevent Injury
The loftier the building, the deeper the foundation must be laid. -- Thomas à Kempis
CDC, more than 27 percent of Americans over the age of forty-five report suffering from chronic pain, and about 10 to 12 percent say that pain has limited their activities on "most days or every day" during the previous six months.
Most "acute" injuries, such as a torn ACL or a hamstring tear, are rarely sudden.
While their onset may be rapid -- instantaneous back or neck or knee pain -- there was likely a chronic weakness or lack of stability at the foundation of the joint
Postural Restoration Institute (PRI)
We run our patients through a series of respiration and movement tests to get the full picture of their respiration strategy and how it relates to their strength and stability issues.
HYPERINFLATED. This person is an upper-chest breather who tends to pull up into spinal extension for both respiration and stability.
In DNS, you learn to think of the abdomen as a cylinder, surrounded by a wall of muscle, with the diaphragm on top and the pelvic floor below.
When the cylinder is inflated, what you’re feeling is called intra-abdominal pressure, or IAP.
Learning to fully pressurize the cylinder, by creating IAP, is important to safe movement because the cylinder effectively stabilizes the spine.
One key test in our movement assessment is to have our patients stand with one foot in front of the other and try to balance. Now close your eyes and see how long you can hold the position.
Ten seconds is a respectable time; in fact, the ability to balance on one leg at ages fifty and older has been correlated with future longevity, just like grip strength.
The spine has three parts: lumbar (lower back), thoracic (midback), and cervical (neck) spine.
Extremely slowed-down, controlled Cat/Cow sequence, moving so slowly and deliberately from one end of your spine to the other that you can feel each individual vertebra changing position,
The point of this exercise is not how much extension or flexion you can reach in extreme Cat or Cow but rather how much segmental control you can achieve, going from one extreme to the other. You should learn to feel the position of each vertebra,
CHAPTER 14 Nutrition 3.0 You Say Potato, I Say "Nutritional Biochemistry"
Religion is a culture of faith; science is a culture of doubt. -- Richard Feynman
Thanks to the poor quality of the science, we actually don’t know that much about how what we eat affects our health.
Simple questions that we posited in chapter 10:
- Are you undernourished, or over
- Are you undermuscled, or adequately muscled?
- Are you metabolically healthy or not?
We need to find ways to get them to consume fewer calories while also increasing their protein intake, and to pair this with proper exercise.
Any dietary intervention that compromises muscle, or lean body mass, is a nonstarter -- for both the under- and overnourished groups.
Wearing a cast on a broken bone will allow it to heal. Wearing a cast on a perfectly normal arm will cause it to atrophy.
Few basic rules: don’t eat too many calories, or too few; consume sufficient protein and essential fats; obtain the vitamins and minerals you need; and avoid pathogens like E. coli and toxins like mercury or lead.
Beyond that, we know relatively little with complete certainty.
What We Sort of Know About Nutritional Biochemistry (and How We Sort of Know It)
So do red and processed meats actually cause cancer or not? We don’t know, and we will probably never get a more definitive answer, because a clinical trial testing this proposition is unlikely ever to be done. Confusion reigns.
One of the best, or least bad, clinical trials ever executed seemed to show a clear advantage for the Mediterranean diet
CHAPTER 15 Putting Nutritional Biochemistry into Practice How to Find the Right Eating Pattern for You
My doctor told me to stop having intimate dinners for four. Unless there
are three other people. -- Orson Welles
The elements that constitute the SAD are almost as devastating to most people as tobacco when consumed in large quantities, as intended: added sugar, highly refined carbohydrates with low fiber content, processed oils, and other very densely caloric foods.
Almost everything we eat, aside from fresh vegetables, is processed to some degree.
For example, cheese is a processed food, invented as a way to preserve milk,
What we’re really talking about, when we talk about the SAD, is junk food.
Once you strip away the labels and the ideology, almost all diets rely on at least one of the following three strategies
- CALORIC RESTRICTION, or CR: eating less in total, but without attention to what is being eaten or when it’s being eaten
- DIETARY RESTRICTION, or DR: eating less of some particular element(s) within the diet (e.g., meat, sugar, fats)
- TIME RESTRICTION, or TR: restricting eating to certain times, up to and including multiday fasting
Tl;dr: From the standpoint of pure efficacy, CR or caloric restriction is the winner, hands down.
This is how bodybuilders shed weight while holding on to muscle mass,
The catch is that you have to do it perfectly -- tracking every single thing you eat, and not succumbing to the urge to cheat or snack -- or it doesn’t work.
DR or dietary restriction is probably the most common strategy employed for reducing energy intake.
Saying you’re going on the "no lettuce" diet is pretty much doomed to fail. And you can still overeat while adhering perfectly to a particular DR,
TR or time restriction -- also known as intermittent fasting -- is the latest trend
In some ways I think it’s the easiest.
But this can still backfire if you overeat.
But the more significant downside of this approach is that most people who try it end up very protein deficient
One not uncommon scenario that we see with TR is that a person loses weight on the scale, but their body composition alters for the worse: they lose lean mass
CR: Calories Matter
If we take in more energy than we require, the surplus ends up in our adipose tissue, one way or another.
If this imbalance continues, we exceed the capacity of our "safe" subcutaneous fat tissue, and excess fat spills over into our liver, our viscera, and our muscles,
One slight advantage is that calorie counting is agnostic to food choices; you can eat whatever
You can lose weight on a restricted-calorie diet consisting only of Snickers bars, but you will feel much better if you opt for steamed broccoli and chicken breasts instead.
Avoiding diabetes and related metabolic dysfunction -- especially by eliminating or reducing junk food -- is very important to longevity.
There appears to be a strong link between calories and cancer, the leading cause of death in the control monkeys in both studies. The CR monkeys had a 50 percent lower incidence of cancer.
The quality of the food you eat could be as important as the quantity. If you’re eating the SAD, then you should eat much less of it.
Conversely, if your diet is high quality to begin with, and you are metabolically healthy, then only a slight degree of caloric restriction -- or simply not eating to excess -- can still be beneficial.
These two studies suggest that if you are eating a higher-quality diet -- and are metabolically healthy to begin with -- then severe caloric restriction may not even be necessary.
The monkeys teach us that if you are metabolically healthy and not over-nourished, like the NIH animals, then avoiding a crap diet may be all you need.
DR: The Nutritional Biochemistry "Diet"
If you cut out carbohydrates altogether but overdo it on the Wagyu steaks and bacon, you will fairly easily find yourself in a state of caloric excess.
Any form of DR that restricts protein, for example, is probably a bad idea for most people, because it likely also impairs the maintenance or growth of muscle.
Similarly, replacing carbohydrates with lots of saturated fats can backfire if it sends your apoB concentration (and thus your cardiovascular disease risk) sky-high.
Manipulating our four macronutrients: alcohol, carbohydrates, protein, and fat.
Alcohol serves no nutritional or health purpose. drinking alcohol is a net negative for longevity.
Carbohydrates
Carbohydrates are our primary energy source.
In digestion, most carbohydrates are broken down to glucose, which is consumed by all cells to create energy in the form of ATP.
Excess glucose, beyond what we need immediately, can be stored in the liver or muscles as glycogen for near-term use or socked away in adipose tissue (or other places) as fat.
This decision is made with the help of the hormone insulin, which surges in response to the increase in blood glucose.
Now we have a tool to help us understand our own individual carbohydrate tolerance and how we respond to specific foods. This is called continuous glucose monitoring, or CGM,
Typically, my healthy patients need to use CGM only for a month or two before they begin to understand what foods are spiking their glucose (and insulin) and how to adjust their eating pattern to obtain a more stable glucose curve.
The higher their blood glucose, the greater their risk of death -- even in the nondiabetic range of blood glucose.
Another study in 2019 looked at the degree of variation in subjects’ blood glucose levels and found that the people in the highest quartile of glucose variability had a 2.67 times greater risk of mortality than those in the lowest
We want to lower average blood glucose and reduce the amount of variability from day to day and hour to hour.
CGM powerfully activates the Hawthorne effect, the long-observed phenomenon whereby people modify their behavior when they are being watched.
Not everyone needs to restrict carbohydrates; some people can handle more than others, and some have a hard time sticking to severe carbohydrate restriction.
Overall, I like to keep average glucose at or below 100 mg/dL, with a standard deviation of less than 15 mg/dL.
If you eat 150 grams of carbohydrates as a serving of rice and beans in one sitting, that has a different effect than eating the same amount of rice and beans spread out over the day
Everyone tends to be more insulin sensitive in the morning than in the evening, so it makes sense to front-load our carb consumption earlier in the day.
I’ve learned thanks to CGM is about what happens to a patient’s glucose levels during the night.
Stress prompts an elevation in cortisol, which in turn stimulates the liver to drip more glucose into circulation.
Another rule of nutrition, which is that timing is important: If you scarf a large baked potato before working out, it will leave much less of a footprint on your daily glucose profile than if you eat it right before bedtime.
It is important to remember the limitations of CGM -- chiefly, that it measures one variable.
This variable happens to be very important, but it is not the only one.
a bathroom scale will suggest that smoking is good for you because you lost weight.
We also monitor other variables that are relevant to diet, beginning with weight (obviously) but continuing with body composition, the ratios of lean mass and fat mass,
Not all carbs are created equal. The more refined the carb (think dinner roll, potato chips), the faster and higher the glucose spike. Less processed carbohydrates and those with more fiber, on the other hand, blunt the glucose impact.
I try to eat more than fifty grams of fiber per day.
Rice and oatmeal are surprisingly glycemic (meaning they cause a sharp rise in glucose levels), despite not being particularly refined; more surprising is that brown rice is only slightly less glycemic than long-grain white rice.
Fructose does not get measured by CGM, but because fructose is almost always consumed in combination with glucose, fructose-heavy foods will still likely cause blood-glucose spikes.
Timing, duration, and intensity of exercise matter a lot. In general, aerobic exercise seems most efficacious at removing glucose from circulation, while high-intensity exercise and strength training tend to increase glucose transiently, because the liver is sending more glucose into the circulation to fuel the muscles.
Don’t be alarmed by glucose spikes when you are exercising.
A good versus bad night of sleep makes a world of difference in terms of glucose control.
All things equal, it appears that sleeping just five to six hours (versus eight hours) accounts for about a 10 to 20 mg/dL (that’s a lot!) jump in peak glucose response, and about 5 to 10 mg/dL in overall levels.
Stress, presumably, via cortisol and other stress hormones, has a surprising impact on blood glucose, even while one is fasting or restricting carbohydrates.
Nonstarchy veggies such as spinach or broccoli have virtually no impact on blood sugar. Have at them.
Foods high in protein and fat (e.g., eggs, beef short ribs) have virtually no effect on blood sugar (assuming the short ribs are not coated in sweet sauce),
But large amounts of lean protein (e.g., chicken breast) will elevate glucose slightly.
Protein shakes, especially if low in fat, have a more pronounced effect (particularly if they contain sugar, obviously).
Stacking the above insights -- in both directions, positive or negative -- is very powerful. So if you’re stressed out, sleeping poorly, and unable to make time to exercise, be as careful as possible with what you eat.
Protein
Protein and amino acids are the essential building blocks of life. Without them, we simply cannot build or maintain the lean muscle mass that we need.
Unlike carbs and fat, protein is not a primary source of energy. We do not rely on it in order to make ATP, nor do we store it the way we store fat (in fat cells) or glucose (as glycogen).
If you consume more protein than you can synthesize into lean mass, you will simply excrete the excess in your urine
We must obtain nine of the twenty amino acids that we require from our diet, because we can’t synthesize them.
The standard recommendations for daily consumption are a joke.
More than one study has found that elderly people consuming that RDA of protein (0.8 g/kg/day) end up losing muscle mass, even in as short a period as two weeks.
In my patients I typically set 1.6 g/kg/day as the minimum, which is twice the RDA.
The data suggest that for active people with normal kidney function, one gram per pound of body weight per day (or 2.2 g/kg/day) is a good place to start -- nearly triple the minimal recommendation.
The added challenge is that it should not be taken in one sitting but rather spread out over the day to avoid losing amino acids to oxidation
The literature suggests that the ideal way to achieve this is by consuming four servings of protein per day, each at ~0.25 g/lb of body weight.
A six-ounce serving of chicken, fish, or meat will provide about 40 to 45 grams (at about 7 grams of actual protein per ounce of meat),
Most people don’t need to worry about consuming too much protein. It would require an overwhelming effort to eat more than 3.7 g/kg/day
For me and my patients, this works out to four servings, as described, with at least one of them being a whey protein shake.
The protein found in plants is there for the benefit of the plant, which means it is largely tied up in indigestible fiber, and therefore less bioavailable to the person eating it.
Plant protein has less of the essential amino acids methionine, lysine, and tryptophan, potentially leading to reduced protein synthesis.
The same is true of protein supplements. Whey protein isolate (from dairy) is richer in available amino acids than soy protein isolate.
Don’t ignore protein. It’s the one macronutrient that is absolutely essential to our goals.
Fat
Fat is essential, but too much can be problematic both in terms of total energy intake and also metabolically.
While carbohydrates are primarily a source of fuel and amino acids are primarily building blocks, fats are both.
They are very efficient fuel for oxidation (think: slow-burning logs) and also the building blocks for many of our hormones (in the form of cholesterol) and cell membranes.
Also important for the health of our brain, much of which is composed of fatty acids.
On a practical level, dietary fat also tends to leave one feeling more satiated than many types of carbohydrates, especially when combined with protein.
There are (broadly) three types of fats: saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and polyunsaturated fatty acids (PUFA).
"saturated" fat simply has more hydrogen atoms attached to its carbon chain.
Within PUFA, we make one more important distinction, which is to separate the omega-6 from the omega-3 variants (also a chemical distinction having to do with the position of the first double bond).
We can further subdivide omega-3 PUFA into marine (EPA, DHA) and nonmarine sources (ALA).
Salmon and other oil-rich seafood provide the former, nuts and flaxseed the latter.
The key thing to remember -- and somehow this is almost always overlooked -- is that virtually no food belongs to just one group of fats.
Olive oil and safflower oil might be as close as you can get to a pure monounsaturated fat,
But all foods that contain fats typically contain all three categories of fat: PUFA, MUFA, and SFA.
Even a ribeye steak contains a lot of monounsaturated fats.
The default fat state of most of my patients (i.e., their baseline fat consumption when they come to me) works out to about 30–40 percent each of MUFA and SFA, and 20–30 percent PUFA -- and
Within that PUFA group, they are generally consuming about six to ten times more omega-6 than omega-3s and usually scant amounts of EPA and DHA.
We try to boost MUFA closer to 50–55 percent, while cutting SFA down to 15–20 percent and adjusting total PUFA to fill the gap.
We also boost EPA and DHA, those fatty acids that are likely important to brain and cardiovascular health, with marine fat sources and/or supplementation.
We titrate the level of EPA and DHA in our patients’ diets by measuring the amount of each found in the membranes of their red blood cells (RBC), using a specialized but readily available blood test.
Our target depends on a person’s APOE genotype and other risk factors
But for most patients the range we look for is between 8 and 12 percent of RBC membrane composed of EPA and DHA.
Practice typically means eating more olive oil and avocados and nuts, cutting back on (but not necessarily eliminating) things like butter and lard, and reducing the omega-6-rich corn, soybean, and sunflower oils -- while
Also looking for ways to increase high-omega-3 marine PUFAs from sources such as salmon and anchovies.
MUFA seems to be the "best" fat of the bunch (based on PREDIMED and the Lyon Heart study), and after that the meta-analyses suggest PUFA has a slight advantage over SFA. But beyond that, we are on our own.
I tell my patients that on the basis of the least bad, least ambiguous data available, MUFAs are probably the fat that should make up most of our dietary fat mix, which means extra virgin olive oil and high-MUFA vegetable oils.
After that, it’s kind of a toss-up, and the actual ratio of SFA and PUFA probably comes down to individual factors such as lipid response and measured inflammation.
Finally, unless they are eating a lot of fatty fish, filling their coffers with marine omega-3 PUFA, they almost always need to take EPA and DHA supplements in capsule or oil form.
TR: The Case for (and Against) Fasting
While intermittent fasting and eating "windows" have become popular and even trendy in recent years, I’ve grown skeptical of their effectiveness.
There is no denying that some good things happen when we are not eating. Insulin drops dramatically because there are no incoming calories to trigger an insulin response. The liver is emptied of fat in fairly short order.
Fasting over long periods also turns down mTOR, the pro-growth and pro-aging pathway
At the same time, lack of nutrients accelerates autophagy, the cellular "recycling" process that helps our cells become more resilient, and it activates FOXO, the cellular repair genes that may help centenarians live so long.
In short, fasting triggers many of the physiological and cellular mechanisms that we want to see.
So why don’t I recommend it to all my patients? because the scientific literature on fasting is still relatively weak,
I still think it can be useful sometimes, in some patients -- typically the ones with the most severe metabolic dysfunction -- but I am less persuaded that it is the panacea
There are really three distinct categories
First, we have the short-term eating windows
- the trick is that it works only provided you make the feeding window small enough.
- standard 16/8 (sixteen hours of fasting, eight hours to eat) is barely enough for most people,
- Usually a narrower window, such as 18/6 or 20/4, is needed to eke out enough of a caloric deficit.
- Human trials of this eating pattern have failed to find much of a benefit.
- Another drawback is that you are virtually guaranteed to miss your protein target with this approach
Next, we have alternate-day fasting (ADF),
- nuanced research suggests there are some significant downsides.
- One small but revealing study found that subjects on an alternate-day fasting diet did lose weight -- but they also lost more lean mass (i.e., muscle) than subjects who simply ate 25 percent fewer calories every day.
Prolonged fasting
- I have become convinced that frequent, prolonged fasting may be neither necessary nor wise for most patients. The cost, in terms of lost lean mass (muscle) and reduced activity levels, simply does not justify whatever benefits it may bring.
Most people can’t safely lose muscle mass, so fasting is a tool that we can only really use in extremis, when there are no other viable options.
Conclusion: Stop overthinking nutrition so much. Put the book down. Go outside and exercise.
CHAPTER 16 The Awakening How to Learn to Love Sleep, the Best Medicine for Your Brain
Each night, when I go to sleep, I die. And the next morning, when I wake
up, I am reborn. -- Mahatma Gandhi
We now know that even one sleepless night can create a state that is the functional equivalent of being legally drunk.
Many studies have found powerful associations between insufficient sleep (less than seven hours a night, on average) and adverse health outcomes: ranging from increased susceptibility to the common cold to dying of a heart attack.
Poor sleep dramatically increases one’s propensity for metabolic dysfunction, up to and including type 2 diabetes, and it can wreak havoc with the body’s hormonal balance.
Good sleep, in terms of not only quantity but quality, is critical to our cognitive function, our memory, and even our emotional equilibrium.
Growing body of evidence that sleeping well is essential to preserving our cognition as we age and staving off Alzheimer’s disease.
Why would evolution allow us to spend up to a third of our lives in a state of unconsciousness, where we could easily be killed or eaten?
We need to sleep about seven and a half to eight and a half hours a night.
There is even some evidence, from studies conducted in dark caves, that our eight-ish-hour sleep cycle may be hard-wired to some extent, suggesting that this requirement is non-negotiable.
Getting significantly less sleep than this, or significantly more, will almost inevitably cause problems in the long run.
A 2014 observational study found that young athletes who slept less than six hours per night were more than two and a half times more likely to experience an injury than their peers who slept eight hours or more.
Devastating effect that poor sleep is having on our energy levels and our performance.
We come to accept the resulting state of mild exhaustion and mental fog as a new normal, a process called "baseline resetting."
It’s like, a regular TV looks fine if that’s all you’ve ever seen. But once you see a 4K screen, you realize that your old cathode-ray tube TV was not very clear after all. The difference is that dramatic.
Old-Man Blood
Kirk Parsley observed this when he was a physician to the SEALs.
Outwardly, these men appeared to be prime physical specimens, finely honed by their rigorous training.
But when Parsley analyzed their blood tests, he was shocked: many of these young guys had the hormone levels and inflammatory markers of men several decades older than them -- "old-man blood,"
Sleep researcher Eve van Cauter of the University of Chicago subjected healthy young people to severely restricted sleep, just 4.5 hours a night, and found that after four days they had the elevated insulin levels of obese middle-aged diabetics and, worse yet, approximately a 50 percent reduction in their capacity for glucose disposal.
Long sleep is also a sign of problems. People who sleep eleven hours or more nightly have a nearly 50 percent higher risk of all-cause mortality, likely because long sleep = poor quality sleep, but it may also reflect an underlying illness.
When we sleep poorly, we can be desperately, irrationally hungry the next day, and more likely to reach for high-calorie and sugary foods than their healthy alternatives.
Sleep and the Brain
Research, however, has pointed to chronic bad sleep as a powerful potential cause of Alzheimer’s disease and dementia.
When we get into bed and close our eyes, a series of physiological changes begins
- Our heart rate slows,
- our core temperature drops,
- our breathing becomes regular
We sleep in a series of well-defined stages, each of which has a specific function and a specific electrical brain wave "signature,"
Normally, our descent is quite rapid: we plunge into the depths, passing through a period of light sleep before dropping into deep sleep.
This sleep stage is called non-REM, or NREM, sleep, and it comes in two strengths, light NREM and deep NREM.
The latter is the more important of the two, especially for neurological health.
As we descend into deep sleep, our brain waves slow until they reach an extremely low frequency, a chanting rhythm of about one to four cycles per second.
This deep sleep dominates the first half of the night, although we typically cycle back and forth between deep and lighter NREM.
Later in the night, typically, our "submersible" rises back up toward the surface, into a zone called rapid eye movement (REM) sleep.
We will cycle between these sleep stages. These sleep cycles last about ninety minutes, and we may even wake up momentarily in between
Deep sleep is when the brain clears out its cache of short-term memories in the hippocampus and selects the important ones for long-term storage in the cortex,
When we are young, REM sleep is important in helping our brains grow and develop.
In adulthood, our REM sleep time tends to plateau, but it remains important, especially for creativity and problem solving.
Another very important function of REM sleep is to help us process our emotional memories, helping separate our emotions from the memory of the negative (or positive) experience that triggered those emotions.
This is why, if we go to bed upset about something, it almost always seems better in the morning.
We remember the event but (eventually) forget the pain that accompanied it.
If this sounds like PTSD, you are correct: studies of combat veterans found that they are less able to separate memories from emotions, precisely due to their lack of REM sleep.
REM-deprived study subjects interpreted even friendly or neutral expressions as menacing.
Deep sleep, on the other hand, seems to be essential to the very health of our brain as an organ.
In deep sleep, the brain activates a kind of internal waste disposal system that allows cerebrospinal fluid to flood in between the neurons and sweep away intercellular junk;
People who have generally slept less than seven hours per night, over decades, tend to have much more amyloid-beta and tau built up in their brains than people who sleep for seven hours or more per night.
Tau, the protein that collects in "tangles" inside unhealthy neurons, is itself correlated to sleep disturbances in cognitively normal people and in those with MCI, or mild cognitive impairment, an early stage of dementia.
Up to half of people with Alzheimer’s disease develop sleep apnea.
One study linked poor sleep quality in cognitively normal people with the onset of cognitive impairment -- just one year later.
Successfully treating sleep disturbance may delay the age of onset into MCI -- by about eleven years, according to one study -- and
It is not enough merely to spend time in bed; good-quality sleep is essential to long-term brain health.
Our ability to obtain deep sleep declines with age, beginning as soon as our late twenties or early thirties, but worsening as we enter middle age.
One possible contributor to this age-related reduction in deep sleep is changes in growth hormone secretion.
Growth hormone is typically released in a pulse about one hour after we begin to sleep at night,
On the other hand, inhibiting growth hormone reduces deep sleep, so it’s not clear which is cause or effect here.
More research points to the forties and sixties as the decades of life when deep sleep is especially important for the prevention of Alzheimer’s disease.
Assessing Your Sleep
Currently, the US sleep medication market is estimated to be worth about $28 billion a year.
But the number of prescriptions has actually been declining recently, perhaps because consumers are catching on to the fact that, by and large, these medicines do not actually work very well.
Sleep medications such as Ambien and Lunesta do not promote healthy, long-lasting sleep so much as they tend to promote a sleep-like state of unconsciousness that does not really accomplish much if any of the brain-healing work of either REM or deep sleep.
If they are using such drugs regularly, it becomes our highest priority to get them off these sleep aids and have them begin to learn to sleep correctly without them.
One drug that we do find helpful for assisting with sleep is trazodone, we typically use it at much lower doses, from one hundred milligrams down to fifty milligrams or even less;
(We have also had good results with the supplement ashwagandha.)
But there are some fairly effective things you can do to improve your ability to fall asleep and stay asleep -- and,
Keep in mind, however, that these tips and strategies are not going to be effective if you have a true sleep disorder, such as insomnia or sleep apnea
The first step
We must renounce our "addiction" to chronic sleep deprivation and admit that we need more sleep, in sufficient quality and quantity.
The next step is to assess your own sleep habits. There are numerous sleep trackers
Measuring variables such as heart rate, heart rate variability (HRV), movement, breathing rate, and more.
In parallel, you should make a longer-term assessment of your sleep quality over the last month.
The best-validated sleep questionnaire is the Pittsburgh Sleep Quality Index,
Another, even simpler quiz called the Epworth Sleepiness Scale,
Another helpful screening tool is the Insomnia Severity Index,
Different people may have widely differing "chronotypes," which is a fancy way of saying that someone is a "morning person"
Others naturally tend to wake up later (and go to sleep later), not really hitting their stride until sometime in the afternoon.
It is important to rule out -- or rule in -- the possibility of obstructive sleep apnea, which is surprisingly prevalent yet underdiagnosed.
Another questionnaire, called STOP-BANG, that correlates pretty strongly with the formal apnea test.
Sleep apnea is a serious medical problem that can have implications for cardiovascular health and dementia risk.
Sleeping Better
Most important, you must create an environment for yourself that is conducive to sleeping well.
Light is the enemy of sleep, Not only does non-natural lighting interfere with our natural circadian rhythm, but it also blocks the release of melatonin,
LED household lighting, which is predominantly on the blue end of the spectrum, meaning it more resembles daylight.
When our brain detects that blue light, it thinks it is daytime and that we should be awake,
A couple of hours before you go to bed, begin turning off unnecessary lights in your house, gradually reducing your light exposure
The devices we stare at before bed -- phones, laptops, video games -- are even worse for our sleep.
Not only do they bombard us with more blue light, but they also activate our minds
The more interactive devices subjects used during the hour before bedtime, the more difficulties they had
Passive devices such as TV, electronic music players, and, best of all, books were less likely to be associated with poor sleep.
Watching TV before bed does not seem to affect sleep quite as negatively as playing video games or scrolling social media does,
Turn off the computer and put away your phone at least an hour before bedtime.
Try to keep your bedroom cool -- around sixty-five degrees Fahrenheit seems to be optimal.
A warm bath before bed may actually help with this process, not only because the bath itself is relaxing but also because when we get out of the bath and climb into our cool bed, our core temperature drops,
Cut back on alcohol -- or better yet, give it up entirely. The effects of alcohol on memory and cognition are apparent even in moderate drinkers.
Students who drank heavily two days after a bout of learning or study forgot or failed to retain most of what they had learned.
Most people think of caffeine as a stimulant that somehow gives us energy, but actually it functions more as a sleep blocker.
It works by inhibiting the receptor for a chemical called adenosine, which normally helps us go to sleep every night.
Over the course of the day, adenosine builds up in our brain, creating what scientists call "sleep pressure," or the drive to sleep.
The half-life of caffeine in the body is up to six hours. Everyone differs in their caffeine tolerance, based on genes and other factors. (23andMe tests for one common caffeine-related gene).
Taking a nap during the day, while sometimes tempting, can also relieve too much of that sleep pressure, making it harder to fall back asleep at night.
To help cultivate sleep pressure is via exercise, particularly sustained endurance exercise (e.g., zone 2), ideally not within two or three hours of bedtime.
It is also important to mentally prepare ourselves for sleeping.
For me, this means avoiding anything that might create stress or anxiety, such as reading work emails or especially checking the news.
If there’s a burning issue that I can’t get off my mind, I’ll write a few lines about it, creating a plan of action for the next morning.
Another way to turn down the sympathetic nervous system and prepare the brain for sleep is through meditation.
How to Improve Your Sleep
Don’t drink any alcohol,
Don’t eat anything less than three hours before bedtime -- and ideally longer. It’s best to go to bed with just a little bit of hunger
Abstain from stimulating electronics, beginning two hours before bed.
For at least one hour before bed, if not more, avoid doing anything that is anxiety-producing or stimulating, such as reading work email or, God help you, checking social media.
For folks who have access, spend time in a sauna or hot tub prior to bed.
The room should be cool, ideally in the midsixties. The bed should be cool too.
Darken the room completely. Make it dark enough that you can’t see your hand in front of your face with your eyes open, if possible. If that is not achievable, use an eye shade.
Give yourself enough time to sleep -- what sleep scientists call a sleep opportunity. This means going to bed at least eight hours before you need to wake up, preferably nine.
Fix your wake-up time -- and don’t deviate from it, even on weekends. If you need flexibility, you can vary your bedtime,
Don’t obsess over your sleep, especially if you’re having problems.
But what if we still can’t sleep? This brings us to the last and most vexing sleep problem, true insomnia.
Stop fighting it. Get up, go into another room and do something relaxing.
Fix a cup of tea (noncaffeinated, obviously), and read a (preferably boring) book until you feel sleepy again.
Find something that is relaxing and enjoyable but that serves no function;
You might not actually have insomnia; you might simply be a night-owl chronotype,
So adjust your bedtime and waking time, if possible.
If the sleeplessness persists,
The most effective treatment is a form of psychotherapy called Cognitive Behavioral Therapy for Insomnia, or CBT-I.
CHAPTER 17 Work in Progress The High Price of Ignoring Emotional Health
Every man is a bridge, spanning the legacy he inherited and the legacy he
passes on. -- Terrence Real
"Religion is for people who are afraid of Hell. Spirituality is for people who have been there."
Emotional health and physical health are closely intertwined,
Suicide, which ranks among the top ten causes of death across all age groups,
Ken Baldwin, who leaped off the Golden Gate Bridge in 1985, when he was twenty-eight, he survived. As he fell, he later told the author Tad Friend, "I instantly realized that everything in my life that I’d thought was unfixable, was totally fixable -- except for having just jumped."
CDC estimates that more than one hundred thousand Americans died from drug overdoses between April 2020 and April 2021, about as many as died from diabetes.
Nothing else about longevity is really worth much without some degree of happiness, fulfillment, and connection to others.
Misery and unhappiness can also destroy your physical health, just as surely as cancer, heart disease, neurodegenerative disease, and orthopedic injury.
The words of my therapist, Esther Perel, rang in my head practically every day: "Why would you want to live longer if you’re so unhappy?"
One framework that the therapists at the Bridge work with, and that I found helpful, is called the Trauma Tree.
The idea behind it is that certain undesirable behaviors that we manifest as adults, such as addiction and uncontrolled anger, are actually adaptations to the various types of trauma we suffered in childhood.
Trauma generally falls into five categories:
- abuse (physical or sexual, but also emotional or spiritual);
- neglect;
- abandonment;
- enmeshment (the blurring of boundaries between adults and children)
- witnessing tragic events
Therapists at the Bridge were careful to explain that there can be "big-T" trauma or "little-t" traumas.
Being a victim of rape would qualify as a big-T trauma, while having an alcoholic parent might subject a child to a host of little-t traumas
Both types can do tremendous damage, but little-t trauma is more challenging to address -- in part, I suspect, because we are more inclined to dismiss it.
Trauma, big T or little t, means having experienced moments of perceived helplessness. The situations in question may or may not have been life-or-death, he explained, "but to a child with an undeveloped brain, it may have seemed that way
I am not suggesting that it is ideal for children to grow up without experiencing any adversity at all, which sometimes seems to be a primary goal of modern parenting
Pretty good litmus test: Would I want my child to experience it?
If my daughter finished dead last in a cross-country race (for example), and didn’t get a medal, that would be okay. Sure, she might feel upset in the moment, but it could also motivate her to train harder and give her a better appreciation for the joy of placing in the top three some day.
What would not be okay is if I had then screamed at her, in front of the other runners, for getting beaten by the shortest kid on the team
A 2019 study provides an elegant demonstration of the principle that setbacks can be a net positive.
The researchers looked at junior scientists who had applied for NIH grants and seperated them into 2 groups
One group had scored just above the threshold for funding, while the other had scored just below the funding line
While the near-miss group were more likely to drop out of science in the immediate aftermath, those who stuck with it eventually outperformed their peers who received funding on their first try
The most important thing about childhood trauma is not the event itself but the way the child adapts to it
Children are remarkably resilient, and wounded children become adaptive children
The problems begin when these adaptive children grow up to become maladaptive, dysfunctional adults
This dysfunction is represented by the four branches of the trauma tree
- addiction, not only to vices such as drugs, alcohol, and gambling, but also to socially acceptable things such as work, exercise, and perfectionism
- codependency, or excessive psychological reliance on another person
- habituated survival strategies, such as a propensity to anger and rage
- attachment disorders, difficulty forming and maintaining connections or meaningful relationships with others
All of this is highly individual; everyone responds and adapts to trauma in a unique way
Medicine 2.0 is set up to treat mental and emotional health in pretty much the same way that it treats everything else: diagnose, prescribe, and, of course, bill.
This is primarily a disease-based model, which is how Medicine 2.0 addresses and solves other problems,
We are more interested in emotional health, which incorporates mental health but is also much broader -- and less easy to codify and categorize.
Our Medicine 3.0 thesis is that if we address our emotional health, and do so early on, we will have a better chance of avoiding clinical mental health issues such as depression and chronic anxiety -- and our overall health will benefit as well.
Esther suggested that I read Terrence Real’s book I Don’t Want to Talk About It, a groundbreaking treatise on the roots of male depression.
His main thesis is that with women, depression is generally overt, or obvious, but men are socialized to conceal their depression, channeling it inward or into other emotions, such as anger, without ever wanting to discuss it.
"90% of male rage is helplessness masquerading as frustration."
As is the case with many men, I had flipped that shame into a feeling of grandiosity.
"Shame feels bad; grandiosity feels good," he told me. "It is central to
masculinity and traditional manhood, this flip from the one-down victim to
the one-up avenger. What’s devilish about flipping from shame into
grandiosity like this is that it works. It makes you feel better in the
short run, but it just creates havoc in your life in the long run."
At the Bridge, I learned that children don’t respond to a parent’s anger in a logical way. If they see me screaming at a driver who just cut me off, they internalize that rage as though it were directed to them.
Second, trauma is generational, although not necessarily linear.
As Terry had written: "Family pathology rolls from generation to generation like a fire in the woods taking down everything in its path until one person, in one generation, has the courage to turn and face the flames. That person brings peace to his ancestors and spares the children that follow."
Reframing is basically the ability to look at a given situation from someone else’s point of view -- literally
This is an incredibly difficult thing for most of us to do, as David Foster Wallace explained in his now famous 2005 commencement address to the graduating class at Kenyon College, "This Is Water":
Everything in my own immediate experience supports my deep belief that I am the absolute center of the universe; the realest, most vivid and important person in existence. We rarely think about this sort of natural, basic self-centeredness because it’s so socially repulsive. But it’s pretty much the same for all of us. It is our default setting, hard-wired into our motherboards at birth.
Think about it: there is no experience you have had that you are not the absolute center of. The world as you experience it is there in front of YOU or behind YOU, to the left or right of YOU, on YOUR TV or YOUR monitor. And so on. Other people’s thoughts and feelings have to be communicated to you somehow, but your own are so immediate, urgent, real.
Easier described than accomplished, reframing entails taking a step back from a situation and then asking yourself, What does this situation look like through the other person’s eyes? How do they see it? And why is your time, your convenience, or your agenda any more important than theirs?
You realize that you have to step back from a situation, temper your reflexive reaction, and try to see what is actually happening.
David Brooks’s book The Road to Character.
Brooks makes a key distinction between "résumé virtues," meaning the accomplishments that we list on our CV, our degrees and fellowships and jobs, versus "eulogy virtues," the things that our friends and family will say about us when we are gone.
Even as I worked on my relationships with those closest to me, I still had a major blind spot: my relationship with myself.
My deep self-hatred and loathing still contaminated most of my thoughts and emotions, and I didn’t even realize it -- nor did I understand why it was happening.
I was speaking with a patient of mine once, an incredibly successful and well-known person, and he said something that stunned me. "I need to be great," he said, "in order to feel like I’m not worthless."
I was assigned to write out a list of forty-seven affirmations, representing one positive statement about myself for each year of my life.
The tools that I use, derive from a school of psychology known as dialectical behavior therapy, or DBT,
Based on the principles of cognitive behavioral therapy, which seeks to teach patients new ways of thinking about or acting on their problems, DBT was developed to help individuals with more serious and potentially dangerous issues,
One thing I like about DBT is that it is backed up by evidence: clinical trials have found it to be effective in helping suicidal and self-harming patients stop their dangerous behavior.
Practicing DBT means literally working through a workbook with a DBT therapist, doing exercises every day.
The practice of DBT is predicated on learning to execute concrete skills, repetitively, under stress, that aim to break the chain reaction of negative stimulus → negative emotion → negative thought → negative action.
DBT consists of four pillars joined by one overarching theme.
- The overarching theme is mindfulness, which gives you the ability to work through the other four:
- emotional regulation (getting control over our emotions),
- distress tolerance (our ability to handle emotional stressors),
- interpersonal effectiveness (how well we make our needs and feelings known to others),
- self-management (taking care of ourselves, beginning with basic tasks like getting up in time to go to work
practicing mindfulness meditation
I did begin to develop occasional flashes of insight, moments when I was able to detach myself from my thoughts and emotions.
It’s not complete detachment in the sense that we’re checking out, but we want to create enough of a gap between stimulus and response so that we are not simply reacting reflexively to things that happen,
That gap, in turn, allows us to process the situation in a calmer and more rational way.
Mindfulness helps us reframe it: The other driver may be rushing to the hospital with a sick child, for all we know.
Another way in which mindfulness helps is by reminding us that when we are suffering, it is rarely because of some direct cause,
Much more often, it is because we are thinking about some painful event that occurred in the past or worrying about something bad that may occur in the future.
the Buddha, who said that "your worst enemy cannot harm you as much as your
own unguarded thoughts."
Seneca improved on that in the first century AD, observing that "we suffer
more often in imagination than in reality."
And later, in the sixteenth century, Shakespeare’s Hamlet noted, "There is
nothing either good or bad, but thinking makes it so."
One obvious way this applies is in how we think about ourselves. What does our inner dialogue sound like? Is it kind and forgiving and wise, or is it harsh and judgmental,
I would record voice memos to myself on my phone, after I did anything that could produce self-judgment,
My instinct in these situations was typically to scream at myself for failing somehow.
My therapist at PCS told me to imagine instead that my best friend had performed exactly as I had done. How would I speak to him?
Another important goal of DBT is to help people learn to regulate their emotions.
DBT teaches a variety of techniques to enable people to maintain and improve their distress tolerance, and to recognize and cope with their emotions -- and not be controlled by them,
One simple tactic that I use to cope with mounting emotional distress is inducing an abrupt sensory change -- typically, by throwing ice water on my face or, if I’m really struggling, taking a cold shower or stepping into an ice bath.
This simple intervention stimulates an important cranial nerve, the vagus nerve, which causes our heart rate and respiratory rate to slow and switches us into a calm, parasympathetic mode (and out of our fight-or-flight sympathetic mode).
Another technique I have grown very fond of is slow, deep breathing: four seconds to inhale, six seconds to exhale. Repeat. As the breath goes, the nervous system follows.
One tactic that I’ve found especially helpful is called opposite action -- that is, if I feel like doing one thing (generally, not a helpful or positive thing), I’ll force myself instead to do the exact opposite. By doing so, I also change the underlying emotions.
I find that spending time moving in nature, simply enjoying the feeling of the wind in my face and the smell of the budding spring leaves (and a heavily loaded pack on my back) helps me cultivate what Ryan Holiday calls "stillness,"
When I’m alone, rucking serves as a mindfulness practice, a kind of walking meditation.
Michael Easter pointed out to me, there is actual research suggesting that exposing oneself to the fractal geometric patterns in nature can reduce physiological stress, and that these effects show up on an EEG.
I complement my therapy sessions by writing in my journal, a place where I can practice articulating my emotions and understanding them, holding nothing back.
I feel strongly that there is no substitute for this kind of work with a trained therapist.
You have to believe you can change -- and that you deserve better.
There’s a quote from Paulo Coelho that I think about often: "Maybe the
journey isn’t so much about becoming anything," he writes. "Maybe it’s
about unbecoming everything that isn’t really you, so you can be who you
were meant to be in the first place."
I wanted to live longer, I think, only because deep down I knew I needed more runway to try to make things right. But I was only looking backward, not forward.
"I think people get old when they stop thinking about the future," Ric told
me. "If you want to find someone’s true age, listen to them. If they talk
about the past and they talk about all the things that happened that they
did, they’ve gotten old. If they think about their dreams, their
aspirations, what they’re still looking forward to -- they’re young."